LA JOLLA, CA—The cornerstone of genetics is the loss-of-function experiment. In short, this means that to figure out what exactly gene X is doing in a tissue of interest—be it developing brain cells or a pancreatic tumor—you somehow cut out, switch off or otherwise destroy gene X in that tissue and then watch what happens. That genetic litmus test has been applied since before people even knew the chemical DNA is what makes up genes. What has changed radically are the tools used by biologists to inactivate a gene.
Until now, scientists wishing to delete a gene in a model organism like a mouse did it by clipping out stretches of DNA encoding entire genes or very big chunks of them from the animal’s genome. This type of gene “knockout” is what La Jolla Institute for Immunology (LJI) investigator Catherine C. Hedrick, Ph.D., used in 2011, when her lab discovered that mice without the gene Nr4a1 lack an anti-inflammatory subtype of white blood cells, nicknamed ‘patrolling monocytes’.
Now, the Hedrick group’s latest study reports a next-generation molecular manipulation aimed at inactivating Nr4a1 in a more precise manner. That study, published in the November 15, 2016, edition of Immunity, reports the loss of the same patrolling monocyte population following inactivation of a molecular switch that turns on Nr4a1. “This new work is exciting, because it shows that we can directly target genes within a specific cell type, which is important for targeted therapies,” says Hedrick, a Professor in the Division of Inflammation Biology.

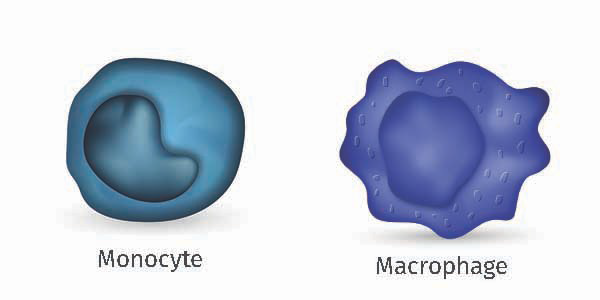
The Hedrick laboratory’s previous demonstration that patrolling monocytes disappear following global Nr4a1 loss proved that the gene is necessary for development of that cell type. Later, her group reported that cancer cells injected into mice lacking Nr4a1 (therefore lacking patrolling monocytes) underwent unchecked metastasis, supporting the idea that patrolling monocytes play anti-cancer roles. But an important experimental question lingered: could the cancer metastasis seen in Nr4a1 knockout mice have anything to do with potential loss of Nr4a1 in a closely related group of cells called macrophages, which use Nr4a1 to control inflammation?
The new paper answers this question by silencing Nr4a1 only in patrolling monocytes. The Hedrick group accomplished this by applying good old-fashioned biochemistry to isolate stretches of DNA that flank the gene and define the on-switch for monocytes. Scientists call tissue-specific gene regulatory elements like this “enhancers.” They then showed that when activated, that DNA region, which they called “enhancer #2” (E2), was capable of switching on Nr4a1 expression only in patrolling monocytes, and not in related cells like macrophages.
The group proved the specificity of the enhancer by engineering mice whose genomes lacked only the E2 enhancer—not the gene itself—and indeed observed a lack of patrolling monocytes. “Until now, we did not have a way to delete a gene only in monocytes without also deleting it in macrophages,” says Graham Thomas, Ph.D., a postdoc in the Hedrick lab and the study’s first author. “Targeting the enhancer allows us to study particular cell types in a highly specific way,” says Thomas. “Also, eliminating enhancers teaches us what turns these genes on in the first place. That knowledge is essential if we are going to design rational targets to go after these cells.”
To confirm that macrophages throw an entirely different molecular switch to turn on Nr4a1, the group exposed mice missing the monocyte E2 switch to a noxious toxin found in bacterial membranes, as a way of seeing whether macrophages can still mount normal inflammatory responses. Indeed, the macrophage response was entirely normal in E2 mutants, unlike the global Nr4a1 “knockout”, showing that macrophages do not use the genetic E2 switch.
Finally, to make sure that E2 enhancer loss mimicked deletion of the entire gene in monocytes the group revisited a tumor model previously used to test Nr4a1’s anti-cancer effect. To do so, they injected melanoma cells into the bloodstream of normal or E2 mutant mice and monitored lung metastasis. Remarkably, outcomes following loss of the switch mirrored what the group had previously observed when they physically removed the gene itself: the lungs of mutant mice contained many more melanoma cells than did lungs of normal mice. This confirmed that the gene regulatory switch is highly specific to one cell type, monocytes and that tumor cell invasion in the absence of this population had nothing to do with deregulated macrophage activity.
Hedrick also thinks the new findings provide new understanding of just how important DNA enhancer regions can be. “Being able to selectively target specific cell types opens up a new world for understanding how to design therapies to treat disease,” she says.
Also contributing from LJI were Richard Hanna, Ph.D., Amy Blatchley, Debbie Yoakum, Sara McArdle, Ph.D., and Zbigniew Mikulski, Ph.D. Other contributors include Neelakantan T. Vasudevan, PhD., and Mukesh Jain, M.D., from Case Western Reserve University in Cleveland; Casey Romanoski, PhD., from the University of Arizona; and Kevin Ross, Bruce Hamilton, Ph.D., and Chris Glass, PhD, all from UCSD.
The study was funded by the National Institutes of Health (R01 HL118765, R01HL134236, R01 CA202987, and R01 GM086912; American Heart Association fellowships 16POST27630002and12DG12070005, and Ruth Kirschstein National Research Service Award (NRSA) and Institutional Predoctoral Training Grant, T32
GM008666, from the National Institute of General Medical Sciences.
About La Jolla Institute
La Jolla Institute for Immunology is dedicated to understanding the intricacies and power of the immune system so that we may apply that knowledge to promote human health and prevent a wide range of diseases. Since its founding in 1988 as an independent, nonprofit research organization, the Institute has made numerous advances leading towards its goal: life without disease®.


