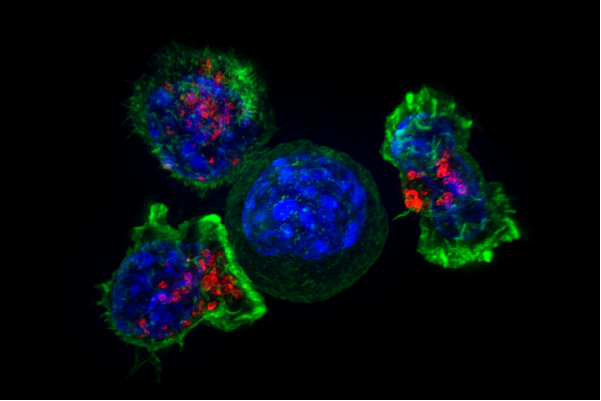
LA JOLLA, CA—One reason we survive into adulthood is that cell-killing T cells usually recognize and eliminate cancerous or pathogen-infected cells. But prolonged overactivity of immune cells summoned to a tumor or infection site can render them useless to dispatch invaders, a cellular state immunologists call “exhaustion.” Fortunately, cancer researchers are devising effective immunotherapies to counter exhaustion and re-motivate immune cells to eradicate a patient’s tumor.
To bolster these approaches, La Jolla Institute for Immunology (LJI) scientists Anjana Rao, Ph.D., and Patrick Hogan, Ph.D., are asking what genes become activated when immune cells flag. Their new study, published in this week’s online issue of Proceedings of the National Academy of Science, reports first that the DNA structure of exhausted T cells differs from that of normal cells. That discovery led them to compile an updated list of candidate DNA binding proteins that may drive exhaustion programs in immune cells. This work provides researchers with additional factors that could be targeted as part of next-generation immunotherapies.
“Immunotherapies are showing real effectiveness in patients, but in some cases effectiveness is short-lived.” says Hogan, a professor in the Division of Signaling and Gene Expression and a study author. “To continue to make real advances in the clinic we must keep refining these approaches. One way we do that is by understanding how tumors talk immune cells out of doing their job.”
To observe how T cells lose their steam in the tumor environment, the team prepared two populations of genetically engineered T-cells: a test group that recognizes a tumor antigen and thus can be rendered non-functional by chronic exposure to the tumor (the exhaustion group), and a control group that remains functional because it doesn’t recognize any tumor antigen. That readied them to compare what goes awry molecularly inside exhausted compared to fully competent T cells.
They did that by injecting the T cells into model mice bearing melanomas to monitor how each test group would behave in a real tumor. Both populations congregated in tumors, but over time cells of the exhaustion group began to display high levels of “exhaustion markers” (as anticipated), because they were overstimulated by the tumor antigen. Among those markers was PD-1, a molecular bad actor notorious for blocking cell-killing capacity of T cells (PD-1 inhibitors, for example, captured headlines two years ago when proven effective against some forms of metastatic melanoma). By contrast, control T cells that the group recovered from a tumor displayed much lower levels of exhaustion markers, simply because they did not perceive the tumor. The next step was to identify genes switched on in the exhausted group and determine how that happened.
To do that the team combined two methods, RNA-sequencing and ATAC-sequencing. RNA-sequencing identifies genes switched on, while ATAC-sequencing identifies genomic regions where the DNA helix is more loosely wound relative to the rest of the genome. Finding these regions provides molecular geneticists with major clues about what’s going on in a cell, as non-compacted DNA generally contains genes undergoing active expression and binds factors that activate those genes.
ATAC-sequencing revealed almost 2000 newly “accessible” regions in failing T cells, a number the group pared down to 450 after subtracting comparable regions in stimulated control T cells. The group then examined the DNA sequence in “exhaustion-related” stretches and deduced, using bioinformatic analysis, what cellular proteins might be recruited to those loci to activate exhaustion-specific gene expression programs.
That analysis revealed the footprints, or binding sites, of many familiar players, one a DNA binding protein called NFAT. “These regions overlapped with regions we previously mapped as NFAT binding sites in T cells chronically exposed to virally-infected cells,” says Hogan. “This could mean that common pathways direct cells toward exhaustion in cancer and chronic infection.”
However, one group of suspects uncovered by the analysis, a family of proteins called Nr4a, had little previous connection with exhaustion in T cells. Further analysis strongly suggested that Nr4a proteins contribute solely to exhaustion, unlike NFAT, which plays a complex, context-dependent role in T cells. The conclusion was clear: DNA binding factors like NFAT and Nr4a proteins likely work in concert to drive T cell dysfunction.
The paper’s lead author, Giuliana Mognol, Ph.D., says the fact that Nr4a proteins appear to function exclusively in T cell exhaustion is a critical finding. “PD-1 inhibitors have produced great results as immunotherapies,” says Mognol, a postdoc in the Hogan laboratory. “Even so, more than 50% of patients do not respond to this therapy. Identifying new molecules that could be targeted together with PD-1 could be important for combination approaches, which are likely the future of immunotherapy.”
One goal of next-gen immunotherapies might be to restore durable immune responses by reversing genomic changes seen in exhausted T cells, possibly by re-compacting DNA that unwinds as T cells become impaired. Whether that’s possible remains unresolved. For example, this paper reports that tumors in melanoma model mice treated with PD-1 blockers shrink as T cell function improves, but that their immune cells showed only minor changes in DNA conformation.
“What we saw in that experiment was a change in cell signaling—not a reversal of structural changes in the T cell genome,” says Hogan. “But I don’t want to be pessimistic and say that’s impossible. Now that we’ve defined what some of those changes are, our next task is to develop tools to reverse them.”
In addition to Rao, Hogan, and Mognol, other authors included LJI scientists Sara Trifari, Ph.D. (now at Sorrento Therapeutics in San Diego), Victor Wong, Ph.D., James Scott-Browne, Ph.D., and Susan Togher; and Roberto Spreafico, Ph.D, and Alexander Hoffmann, Ph.D., of UCLA.
The study was supported by NIH grants R01 AI109842 and AI40127 (to A.R. and P.G.H.) and AI84167 (to P.G.H.). It was also funded by CNPq, Brazil; the QCB Collaboratory community; a Pediatric Hematology-Oncology Fellowship from UCSD; and the Damon Runyon Cancer Research Foundation.
About La Jolla Institute
La Jolla Institute for Immunology is dedicated to understanding the intricacies and power of the immune system so that we may apply that knowledge to promote human health and prevent a wide range of diseases. Since its founding in 1988 as an independent, nonprofit research organization, the Institute has made numerous advances leading towards its goal: life without disease®.