Cancer
One in four deaths in the United States is caused by cancer. According to the U.S. Centers for Disease Control and Prevention, breast and prostate cancers are the most common in the United States and bronchus cancers have the highest death rate.
Cancers all have one thing in common: mutated cells from one’s own body begin to grow uncontrollably. Some cancers are caused by inherited genetic mutations, such as the BRCA gene involved in some breast and ovarian cancers. Other cancers come from random genetic mutations, sometimes caused by environmental contaminants or consumption of alcohol or tobacco. Many cases of cancer come hand-in-hand with other diseases. For example, the intestinal tissue damage caused by Crohn’s disease and ulcerative colitis can also lead to colorectal cancer. Viruses such as human papillomavirus infection (HPV) can also lead to cancer-causing mutations.
The huge range of cancer causes—and organs affected—means there cannot be a single cancer cure. Some cancers can be controlled or killed through surgery, radiation or chemotherapy. More recently, antibody therapies have shown promise in stopping breast cancer growth and lymphomas.
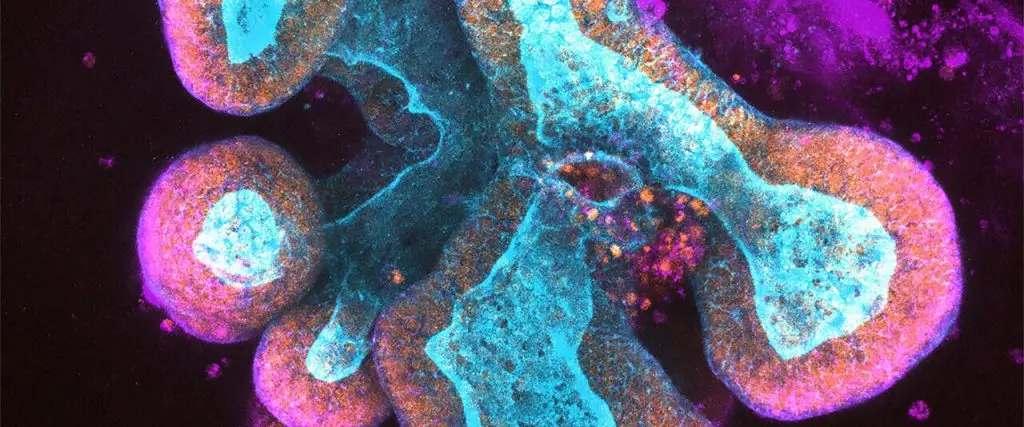
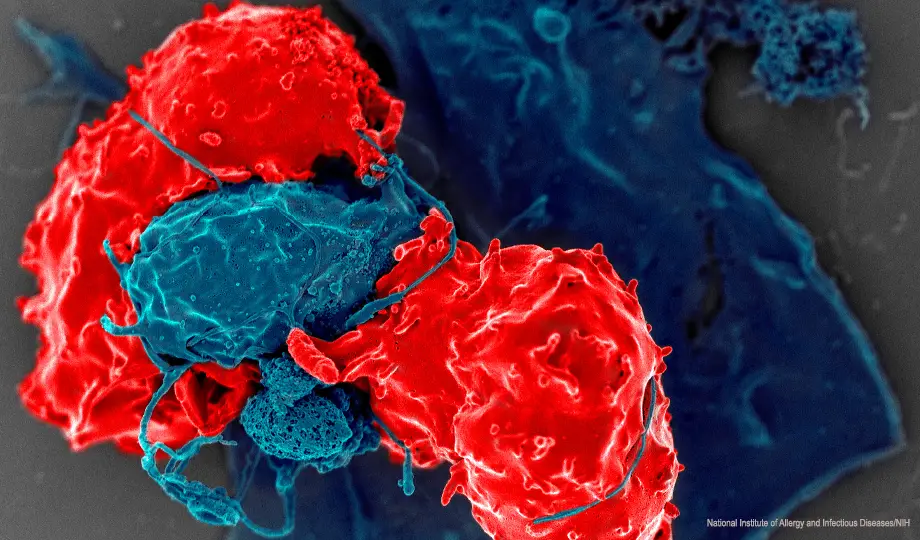
Immune system research can open the door to better detecting and treating all types of cancer. Rather than killing tumor cells directly, immunotherapies rally a patient’s often dormant immune cells to do the job. Key players in immunotherapies are the body’s T cells, also called “the immune system’s warrior cells.”
Cancer immunotherapies save lives every day. Still, many patients fall through the cracks. Either their cancers do not respond to immunotherapies or they have to halt treatment due to toxic side effects.
Our Approach
Scientists in LJI’s Center for Cancer Immunotherapy are committed to making cancer immunotherapies work for more people.
Advancing personalized immunotherapies
LJI Professor Stephen Schoenberger, Ph.D., is working to advance new and more effective personalized immunotherapies. These therapies focus on antigens expressed in a given individual’s tumor and harness the ability of their own immune system to respond. In 2023, Dr. Schoenberger and colleagues published a pair of studies showing how we might harness CD4+ T cells while boosting the cancer-fighting power of CD8+ “killer” T cells. The research team went on to demonstrate a new kind of vaccine design that recruits both types of T cells to destroy large tumors.
In a 2024 study, Dr. Schoenberger and LJI Professor Bjoern Peters, Ph.D., found that many patients thought to have immunologically “cold” tumors (which didn’t spark a strong reaction from immune system defenses) actually do make cancer-fighting T cells. This research opens to door to potentially harnessing this pre-existing natural immunity to boost the immune system’s ability to fight these tumors.
In 2024, LJI Professor Pandurangan Vijayanand, M.D., Ph.D., published an in-depth study into how the immune system’s T cells target pediatric brain tumors. Their research suggests that a small number of pediatric brain tumor patients already have cancer-fighting T cells within their tumors. This discovery, published Nature Cancer, is an important step toward helping identify which pediatric brain tumor patients might benefit from cancer-fighting immunotherapies.
Leading data science and analysis
LJI scientists are also developing invaluable new cancer research tools. One important tool is CEDAR, a new cancer research database developed at LJI. This database is the go-to site for researchers around the world to access data on cancer epitopes, the regions on cancer cells that can be targeted by the immune system. By sharing epitope data, researchers can develop new immunotherapies to target many cancer sites. CEDAR is directed by LJI Professors Alessandro Sette, Dr.Biol.Sci., and Bjoern Peters, Ph.D., and builds upon their experience organizing infectious disease data in a similar database called the Immune Epitope Database (IEDB).
In 2024, LJI Professor Anjana Rao, Ph.D. and LJI Associate Professor Ferhat Ay, Ph.D., shared an important advance in fighting cancer: a new computational method for linking molecular marks on our DNA to gene activity. Their work may help researchers connect genes to the molecular “switches” that turn them on or off. This research, published in Genome Biology, is an important step toward harnessing machine learning approaches to better understand links between gene expression and cancer development.
Studying cancer origins
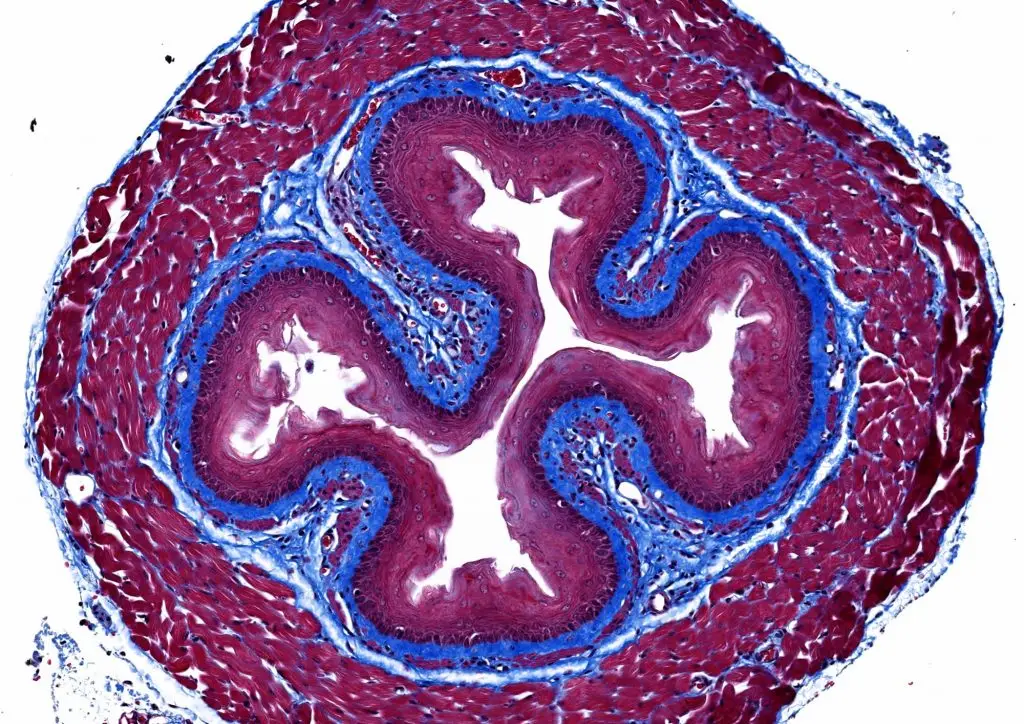
Genetic mutations kick start cancers. Some mutations shuffle the genetic code, but others come from the deletion of key genes. In 2022, Dr. Rao made a major breakthrough in understanding how deletion of the genes that encode TET proteins can lead to cancer growth. This new study, published in Nature Communications, was the first to show the immediate consequences of deleting all three genes from the TET family in mouse embryonic stem cells.
By using a mouse model, Dr. Rao and her colleagues found that TET proteins are critical for keeping the process of cell and DNA replication running smoothly. Without TET proteins, important genes go missing, leading to the mutations, or aneuploidies. Uncovering this direct connection between TET loss of function and aneuploidies gives researchers a clue to how to find genes that underpin cancer development.
Dr. Ay is also investigating the very roots of pediatric blood cancers. LJI Instructor Abhijit Chakraborty, Ph.D., is working to understand how a healthy cell morphs into a cancer cell. He’s shown how a “shattering” of the chromosome, an event called chromothripsis, drives cancer development. Dr. Chakraborty has won funding to study pediatric iAMP21, a rare subtype of B cell leukemia with chromothripsis that leads to aggressive cancer with a high relapse rate.
LJI faculty member and Global Autoimmune Institute Assistant Professor Samuel Myers, Ph.D., is working closely with scientists at Yale University to shed light on mutations in a specific protein that appears to drive intellectual disabilities and potentially the development of certain brain cancers. Dr. Myers’ expertise in proteomics can give us important clues to why seemingly healthy cells go rogue and cause cancer.
Dr. Myers recently shared a new method, published in Nature Methods, to quickly assess the “phosphorylation sites” where phosphate groups attach to proteins and modulate their function. This method makes it easier for scientists study protein modifications with important roles in immune cells—roles such as cancer immunity.
Boosting immune cell defenses
Dr. Rao, and Patrick Hogan, Ph.D., are dedicated to studying a dangerous phenomenon called T cell exhaustion, where T cells stop doing their jobs after trying and failing to kill a tumor. The research team has developed methods to engineer T cells resistant to T cell exhaustion. “The idea is to give the cells a little bit of armor against the exhaustion program,” says LJI Professor Patrick Hogan, Ph.D. “The cells can go into the tumor to do their job, and then they can stick around as memory cells to prevent cancer recurrence.
LJI Professor Sonia Sharma, Ph.D., is changing how we think of the innate immune system’s role in cancer protection. The cells of the innate immune system are the body’s first line of defense, and they can also produce molecules that may affect a patient’s response to cancer immunotherapies. Sharma has worked to uncover the function of small molecules called metabolites. Metabolites do a lot in the body by regulating cellular energetics, but some also work as signaling molecules that “talk” to immune cells.
LJI Professor Michael Croft, Ph.D., studies how small signaling molecules or cytokines collectively called tumor necrosis factor superfamily (TNFSF) proteins and their receptors (TNFRSF), which are expressed on T cells, boost the immune system response in paradoxical settings. Drugs that block TNFSF or TNFRSF proteins are being used successfully in the clinic to suppress immune responses to treat multiple autoimmune or inflammatory diseases. Croft’s lab is investigating the other side of that coin: namely whether TNFRSF modulators can enhance T cell responses in the context of cancer.
LJI Professor Hilde Cheroutre, Ph.D., is also searching for ways to rally anti-tumor T cell responses. Working with researchers at Japan’s RIKEN Institute, she has identified a molecular switch that allows so-called T-helper cells to morph into more aggressive killer T cells capable of attacking either tumors or infected cells. These findings could encourage development of potent drugs targeting cancer, AIDS or other infectious diseases.
LJI Assistant Professor Miguel Reina-Campos is investigating the cancer-fighting power of specialized immune cells called tissue-resident T cells. These T cells have adapted to living in specific organs and are well suited to killing solid tumors that may try to develop in those organs. Dr. Reina-Campus aims to investigate the basis of this T cell immunity to improve life-saving cancer immunotherapies.
A closer look at toxic side effects
Dr. Sharma’s laboratory has found that cancer patients who experience severe side effects during cancer immunotherapy have unusually low levels of a metabolite called LPC. Without LPC, cancer patients develop autoimmune-like conditions after receiving immune checkpoint blockers —some side effects are so bad that they have to stop taking these life-saving treatments. Her experiments, using a humanized mouse model treated with the immune checkpoint blocker Yervoy, suggest researchers may be able to add LPC back into the body to make cancer immunotherapies work better. Dr. Sharma is now working on bringing this concept to the clinic.
Meanwhile, Dr. Vijayanand and his lab members are are investigating why cancer immunotherapies only help a fraction of patients. In early 2022, long-time collaborator and Christian H. Ottensmeier, M.D., Ph.D., FRCP, of LJI and the University of Liverpool, shared the results of their investigation into why an experimental immunotherapy triggered harmful gut inflammation in clinical trial subjects. Their work showed that the immunotherapy allowed a harmful subtype of T cells to move unchecked in the gut. With this knowledge, Drs. Vijayanand and Ottensmeier experimented with using a smaller, slower dosing strategy in a mouse model. Their work suggests tweaking the timing of cancer immunotherapies may spare patients from some side effects.
The Vijayanand Lab is also taking a close look at the immune system reacts when patients are given two kinds of immunotherapy at once: anti-PD-1 therapies and CTLA4 therapies. A 2021 study from the team shows how this strategy may make things worse for some patients. The lab has shown that anti-PD-1 therapies lead to more T follicular regulatory (Tfr) cells in tumors. In a healthy person, Tfr cells do the important job of stopping haywire T cells and autoantibodies from attacking the body’s own tissues. But in a cancer patient, Tfr cells suppress the body’s ability to kill cancer cells. This means anti-PD-1 therapies may cancel out the benefits of CTLA4 therapies.
The researchers think it may be more effective to first use CTLA4 therapy to deplete the Tfr population and then give patients anti-PD-1 therapy to further boost the immune system’s cancer-fighting power. Preliminary data suggest this sequential therapy approach can improve survival outcomes in melanoma patients. Drs. Vijayanand and Ottensmeier are now working to set up new clinical trials to test this sequential approach, and they are collaborating with Cancer Research UK to develop therapeutics that target Tfr cells.
Cancer vaccines
Dr. Schoenberger is also is implementing an immunotherapy strategy that deploys a patient’s own T cells against tumor cells, leaving normal tissues relatively unscathed. The approach is based on the fact that tumor cells exhibit unique mutated proteins on their surface. Dr. Schoenberger, partnering with colleagues at UC San Diego, will employ next-generation DNA sequencing to first identify those “neoantigens” in tumors from patients with head and neck cancer and then isolate pools of patients’ T cells that recognize them. Patients will then be reinfused with their own selected T cells in order to kill cells decorated with the neoantigen. An alternate approach is to create a therapeutic vaccine to stimulate a patient’s immune system to clear cells bearing the marker.
Learn more:
Related News
- Institute News
- Research News
- Institute News
Research Projects
In 2013, Dr. Vijayanand teamed up with Professor Christian Ottensmeier at the Cancer Center, University of Southampton, UK, to set up a large patient-centered cancer immunology program. Our work [...]
Preliminary data from our lab shows that vascular endothelial cells (vECs) mount remarkably potent innate responses to cell-free DNA, which is well in accordance with their role as sentinels of [...]