LA JOLLA, CA—Scientists at La Jolla Institute for Immunology (LJI) are investigating a talented type of T cell.
Most T cells only work in the person who made them. Your T cells fight threats by responding to molecular fragments that belong to a pathogen—but only when these molecules are bound with markers that come from your own tissues. Your influenza-fighting T cells can’t help your neighbor, and vice versa.
“However, we all have T cells that do not obey these rules,” says LJI Professor and President Emeritus Mitchell Kronenberg, Ph.D. “One of these cell types is mucosal-associated invariant T (MAIT) cells.”
Now Kronenberg and his LJI colleagues have uncovered another MAIT cell superpower: MAIT cells can recognize the same markers whether they come from humans or mice. Kronenberg calls this finding “astounding.” “Humans diverged from mice in evolution 60 million years ago,” he says.
This new research, published in Science Immunology, sheds light on the genes and nutrients that give MAIT cells their fighting power. The findings are an important step toward one day harnessing these cells to treat infectious diseases and improve cancer immunotherapies.
“Because MAIT cells are the same across individuals, they could more easily be used in cell therapies, where, in principle, my MAIT cells could be given to you,” says Kronenberg.
The new study also opens the door to exploiting MAIT cells to improve cellular therapies. “If we could make normal T cells more like MAIT cells, maybe we could make them act faster and more vigorously to combat any type of infection or cancer,” says study co-first author Gabriel Ascui, a UC San Diego graduate student in LJI’s Kronenberg Lab.
Why MAIT cells are special
Kronenberg was initially interested in MAIT cells because of their unexpected speed. Typical T cells need a few days to develop in the thymus and adapt to fighting new threats. MAIT cells are much faster because they can respond to more generic markers of infection, rather than hunting for very specific tissue-type markers. For MAIT cells, a red flag is a red flag, no matter who is waving it.
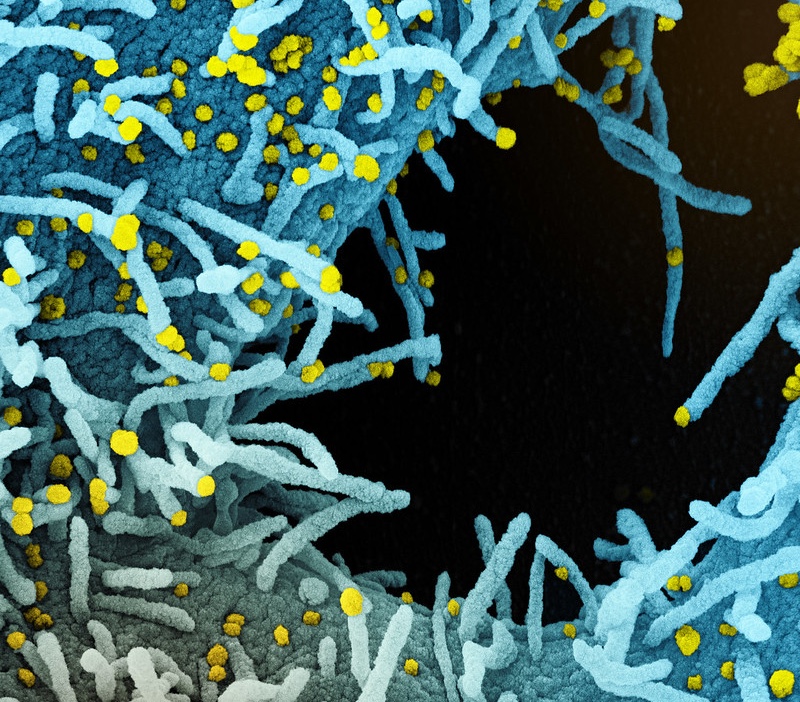
This lack of specificity makes MAIT cells similar to the immune system’s first-responder cells, such as macrophages and neutrophils, which make up the “innate” immune system. “MAIT cells have this ‘innate-like’ characteristic,” says Ascui. “They’re like your first line of defense.” In fact, MAIT cells tend to gather in tissues like the lungs and intestines, where the body is under constant threat from airborne and foodborne pathogens.
The new study shows that MAIT cells don’t just recognize a range of markers within one person. Instead, these odd T cells can “see” markers shared between humans—and even between species. Scientists call these kinds of shared markers “conserved.” There has been no reason for the markers to change over the eons, so they remain the same across related species.
But just because these MAIT cells look the same between species, doesn’t mean they fight pathogens—or make energy—in exactly the same ways.
Why look at mouse cells?
Comparing human and mouse MAIT cells is important for guiding future studies where mice can serve as useful animal models to study exactly how these cells combat pathogens.
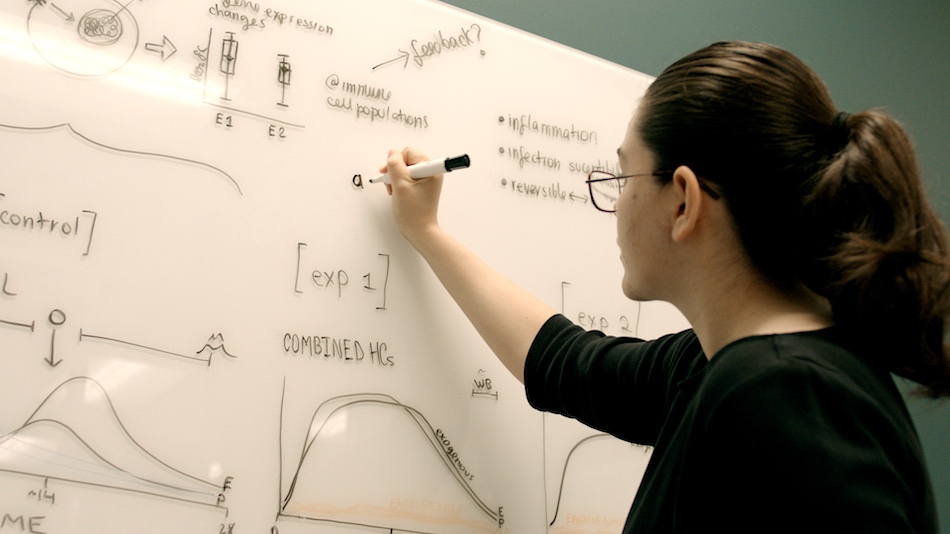
Kronenberg, Ascui, and their colleagues used single-cell sequencing and other tools to compare differences in gene expression pathways between human and mouse MAIT cells. The scientists found that mice have two different kinds of MAIT cells, which produce different inflammatory molecules, called cytokines. One kind of MAIT cell, which the scientists call MAIT1, produces a lot of a cytokine called interferon-gamma. The other kind of the MAIT cell, called MAIT 17, produces a lot of a cytokine called interleukin-17.
These cytokines help the MAIT cells take aim at different threats. MAIT1 cells are better at targeting viruses, while MAIT17 cells are better at targeting bacteria.
The same is true for human MAIT cells. A recent Nature Cell Biology study from the Kronenberg Lab, co-led by LJI Instructor and Immunometabolism Core Director Tom Riffelmacher, Ph.D., shows that human MAIT cells also split into MAIT1 and MAIT17 types.
In the new study, the team found that MAIT cells from both species are more capable of taking up and storing fat, compared with typical T cells. This finding suggests MAIT cells are more dependent on this nutrient for energy. This discovery is also in line with previous work in the Kronenberg Lab showing that some human MAIT cells depend on fat to fight pathogens.
The key difference between the species was that human MAIT cells tend to produce more of their respective cytokines, making them more “defined” than the mouse MAIT1 and MAIT17 cells.
When mice live like us
The scientists needed to know—was this difference in human and mouse MAIT cells linked to genetic differences or to our different habitats? Lab mice, such as those cared for at LJI, are housed in ultra-clean vivariums. Their food is blasted in an autoclave to kill pathogens, and their water, toys, and cages are kept as sterile as possible.
Kronenberg and Ascui were curious—do mice living in less-controlled environments show differences in MAIT cell function? The team collaborated with UC San Diego scientists to study MAIT cells from mice kept in so-called “dirty” conditions, similar to a pet store environment. Their research suggests MAIT cells from these mice have even more in common with human MAIT cells, especially when it came to their MAIT1 cells, which produced more interferon-gamma than lab mouse MAIT1 cells.
“Pet stores aren’t dirty in the conventional sense” says Kronenberg. “But part of the idea is that the ‘dirty’ mice are living in an environment—with more microbes and immune system challenges—that’s a little closer to human environments.”
The team also compared MAIT cells found in different parts of the body, such as the blood, thymus (where T cells, including MAIT cells, develop), and the lung and spleen (where MAIT cells camp out). They discovered that MAIT cells still in the thymus look very similar between humans and mice (“dirty” or not); however, MAIT cells from the lungs and blood are more different between humans and lab mice.
MAIT cells from the “dirty” mice fell between the two groups, adding to the evidence that more natural-like environments change how MAIT cells develop and learn to target disease.
“Environmental, as well as genetic differences, shape the species differences in these cells,” says Kronenberg.
What does this mean for clinical research?
The new study gives scientists a sort of answer key, a list of genetic signatures to tell MAIT cells apart depending on the species and tissues they come from. Going forward, the team is interested in whether they can prompt typical T cells to express similar genetic signatures.
“If we could make normal cells more ‘innate,’ like MAIT cells, perhaps we could improve t cell therapy for cancer,” says Ascui. “That’s one avenue we’re looking at.”
Kronenberg is also interested in whether scientists can modify MAIT cells to actually decrease levels of IL-17 in the body. Although IL17 helps fight infections, some T cells produce IL-17 against the wrong targets, triggering harmful inflammation and even autoimmune disease.
“There are cases where IL-17 can be a bad actor,” says Kronenberg. “So there are cases where we might want to induce more MAIT17 cells, expand their population, but we’d also like to find ways to prevent them from arising in situations where they might not be what we want.”
Additional authors of the study, “Transcriptomes and metabolism define mouse and human MAIT cell populations,” include co-first authors Shilpi Chandra and Thomas Riffelmacher, and Ashu Chawla, Ciro Ramírez-Suástegui, Viankail C. Castelan, Gregory Seumois, Hayley Simon, Mallory P. Murray, Goo-Young Seo, Ashmitaa L. R. Premlal, Benjamin Schmiedel, Greet Verstichel, Yingcong Li, Chia-Hao Lin, Jason Greenbaum, John Lamberti, Raghav Murthy, John Nigro, Hilde Cheroutre, Christian H. Ottensmeier, Stephen M. Hedrick, Li-Fan Lu, and Pandurangan Vijayanand.
This research was supported by the National Institutes of Health (AI105215, AI71922, AI137230, AI108651, AI163813, S10RR027366, S10OD025052, S10-OD016262), the Wellcome Trust (grant 210842_Z_18_Z); UC San Diego Program in Immunology seed grant, the Whittaker Fund, iCURE, and the Wessex Clinical Research Network.
DOI: 10.1126/sciimmunol.abn8531
###