Let’s say you’re unlucky. A virus breaches your body’s first lines of defense. It slips past the mucus traps in your nose and sends your innate immune cells (cells such as dendritic cells, neutrophils, monocytes) into a panic. What happens next?
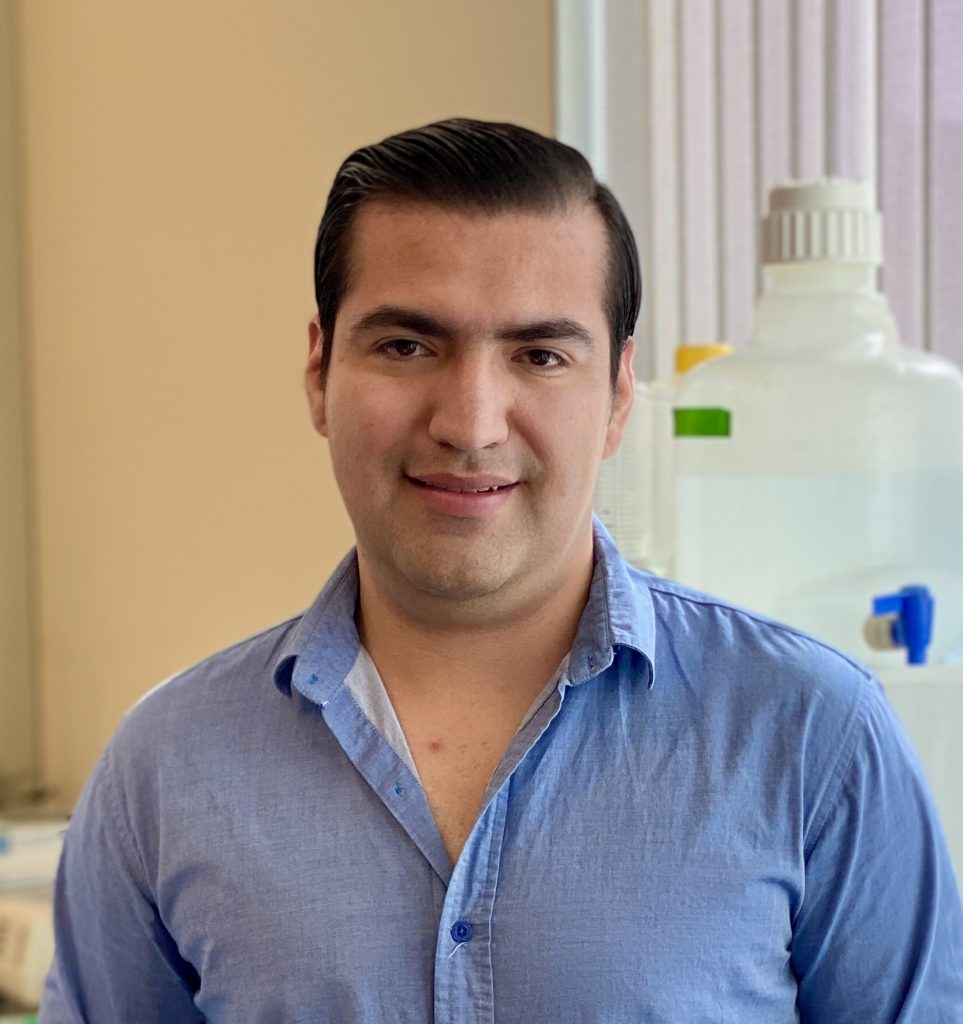
Alba Grifoni, Ph.D., studies how the body’s T cells launch a counterattack. By combining experimental data and bioinformatics tools, Grifoni and her colleagues at La Jolla Institute for Immunology (LJI) have revealed how T cells recognize and target viruses such as SARS-CoV-2 and mpox. Grifoni has earned international honors for these breakthroughs, and she ranked among top scientists on Clarivate’s 2022 “Highly Cited” list.
This year, Grifoni launched her own laboratory as an LJI Research Assistant Professor. In this Q&A, Grifoni shares what her research means for vaccine development.
Q: What is your lab’s mission?
Grifoni: My research is focused on preparedness for emergent viruses. My lab is particularly interested in the question of what happens on the T cell side of things. We know that the immune system uses antibodies, which are made by B cells, and T cells to fight viruses.
You need to consider both T cell and B cell responses in vaccine design. So throughout my career, I have been working on different viral infections—to figure out what part of a virus is recognized by T cells, and I believe this research should always be done in collaboration with B cell researchers.
Q: Our T cells recognize just parts of a virus?
Yes, we call these parts “epitopes,” and related viruses sometimes have epitopes in common. I want to find out how conserved epitopes are within the same viral family. Can we design a “pan” vaccine for a viral family—to include the T cell point of view together with B cells? These vaccines would benefit from inducing a B cell response but also strengthening a person’s T cell response to several related viruses at once.
My SARS-CoV-2 work with LJI Professor Alessandro “Alex” Sette, Dr.Biol.Sci., has made it possible to really speed up T cell epitope research. Finding the shared epitopes between viruses is important because we know that when there’s an emerging disease, we need these answers fast to develop effective vaccines.
Q: Which diseases is your lab tackling first?
I’ve received a PO1 grant from the NIH to collaborate with researcher Michael Diamond, Ph.D., of Washington University, to design a pan-coronavirus vaccine that induces both B and T cells. I have also been working on SARS-CoV-2 viral evolution—specifically in understanding the effect of SARS-CoV-2 variants on T cells. Alex and I are part of the international SARS-CoV-2 Assessment of Viral Evolution (SAVE) consortium. As part of this initiative, I was awarded a one-year grant to look at the effect of “breakthrough” infections on T and B cells. This is a collaboration with Alex (looking at T cells) and Shane Crotty, Ph.D., (looking at B cells), and myself.
That study should be out soon, hopefully. As part of this grant, I am also working to predict the effect of new variants on T cells, and Alex and I have a bioinformatics study that will be released soon on the effect of BA2.86 (pirola) variant.
I’ve also recently been awarded, with Alessandro Sette, funding through the Coalition for Epidemic Preparedness Innovations (CEPI) to collaborate with researchers across the country to study how to stop viruses from the Paramyxovirus and Arenaviruses families, which include Nipah virus and Lassa virus, respectively.
Q: What kinds of tools do you use to uncover T cell epitopes?
We use a combination of experimental and bioinformatic approaches, depending on how much information we already have about the virus. With SARS-CoV-2, for example, we now know a lot about how T cells recognize and target it. But we don’t know as much about other viruses.
So depending on what we know, we can either use the experimental information already available, for example, in the Immune Epitope Database (IEDB), or we can perform bioinformatic prediction analyses. This is when we use bioinformatics tools to come up with a “best guess” for which viral epitopes our T cells might recognize. From there, we can do experiments in the lab to understand which epitopes on the virus are the key T cell targets and how we might incorporate these findings in vaccine design.
Q: Your research has the potential to help so many people around the globe. Could you share the importance of the international scope of your work?
The fact that LJI is very international has facilitated a lot of valuable collaborations. Alex Sette and I collaborated with more than 180 labs throughout the world for our SARS-CoV-2 work. These collaborations are still active, and if we see a new viral outbreak, we can ask, “What are we going to do about it? How can we tackle the problem together as a team?” I think that’s very powerful.
Q: What makes LJI a good place to set up your new lab?
I am personally very excited to grow my career at the Institute. For me, it’s been inspirational to work with my mentor, Alex Sette, and with Shane Crotty. They’ve helped me become more and more independent as the scientist I am now.
To have experts here at LJI who have different interests—but are focused on the same infectious diseases—is really useful. It takes a lot of additional effort to share data, share knowledge between institutions. So to have these experts collaborating internally at LJI shows a great vision at the Institute.
I’d also really like to thank my team! No one is an island, and my lab is really a team of people who put in a lot of effort every day.
Learn more
Family resemblance: How T cells could fight many coronaviruses at once
LJI scientists confirm smallpox vaccine also teaches T cells to fight mpox