When immune cells go haywire in autoimmune disease, they often like to attack a specific organ—and one organ only. For example, in type 1 diabetes, T cells start killing cells in the pancreas.
Lupus is a whole different beast. Lupus is a “systemic” autoimmune disease, which means harmful immune cells cause widespread inflammation and tissue damage. As these immune cells pinball around the body, they can damage the joints, kidneys, skin, brain, and many other organs.
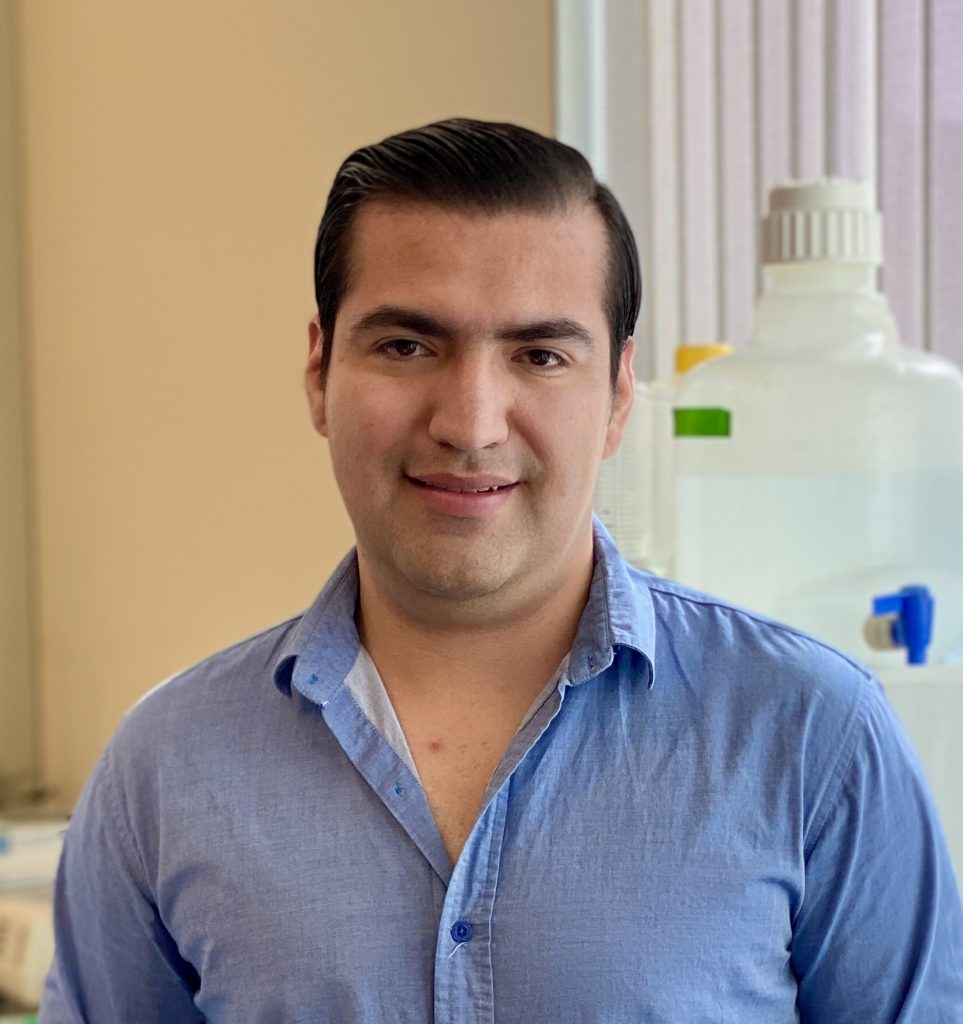
LJI Instructor Carolyn Moderbacher, Ph.D., wants to use lupus’s systemic nature to her advantage. She’s working with lupus patients to hunt down key immune cells in their nasal passages. By swabbing tissues deep within the nose, Moderbacher hopes to uncover exactly how immune cells drive this devastating disease.
Moderbacher’s unusual approach recently won her a Lupus Innovation Award and nearly $450,000 in funding from the Lupus Research Alliance, the world’s largest private funder of lupus research.
“This research could be transformative, and it’s really exciting to have the funding to move it forward,” says Moderbacher, who works in the lab of LJI Professor and Chief Scientific Officer Shane Crotty, Ph.D.
Moderbacher will be the first scientist to use the nasal passages as a window into lupus development. In fact, the deep nasal swab method itself is brand new to the field of immunology. The method was developed at LJI and first described in a 2024 Nature study, in which LJI researchers used the swabs to track immune cell responses to SARS-CoV-2 infections and COVID-19 vaccines.
As the researchers demonstrated, deep nasal swabs are valuable because they reach beyond the nostrils to capture immune cells from lymphoid tissues hidden within the nasal passage, near the back of the throat. These lymphoid tissues are home to special B cell gathering spots, called germinal centers, where B cells learn to make antibodies. Your nasal passages need those antibodies on site to fight potential respiratory infections.
“The Crotty Lab focuses on vaccine and infectious disease-related immunity, but autoimmunity is really just the other side of the same coin,” says Moderbacher. “Instead of trying to get a better response to a vaccine, in autoimmunity you’re trying to dampen an over-exuberant and misdirected immune response.”
Because lupus is a systemic disease, Moderbacher says there’s good reason to think that B cells in the nasal passage might also churn out the “auto-reactive,” or self-targeting antibodies that cause inflammation.
“To understand lupus—and other autoimmune conditions that are mediated by antibodies—you really need to be able to look at the tissues where these autoantibodies are developing. These would be lymphoid tissues, like your lymph nodes,” says Moderbacher. “But these sites aren’t routinely accessed. You might get a sample from a biopsy, but that’s a one-off. You can’t look over time in the same people.”
The nasal swab technique may be the breakthrough Moderbacher has been looking for. Clinical study volunteers with lupus can even come in for routine swabs through LJI’s John and Susan Major Center for Clinical Investigation. Moderbacher can then study if their germinal center cells change over time or show features specific to lupus patients.
“For the first time, we might actually get the ability to sample lymphoid tissue where we think pathogenic, autoreactive cells are living and evolving,” says Moderbacher. “We can then see if we can correlate that immune system activity with disease progression, disease flares, and whether a patient is responding to therapy—or even identify unique biomarkers that could become therapeutic targets.”
For the study, Moderbacher will also search the blood and nasal lymphoid tissues for specific T cells that play a role in lupus development. She is working with T cell experts in the labs of LJI Professor Alessandro Sette, Dr.Biol.Sci., and LJI Research Assistant Professor Alba Grifoni, Ph.D., to develop “peptide pools” to capture these T cells for analysis.
Moderbacher has already started administering nasal swabs to a small number of clinical study volunteers recruited by research partners at UC San Diego. Her preliminary data suggest that researchers can indeed capture key immune cells that may drive lupus.
“We’ve followed a small cohort of a half-dozen individuals and sampled them monthly,” says Moderbacher. “And we’ve been able to reproducibly get the same germinal center cell populations in the same individuals over time—which has been really exciting.”
Moderbacher hopes this lupus project is just the start of a promising area of research. For example, she’s connected with UC San Diego researchers to see how they might use the nasal swab technique to better understand rheumatoid arthritis, another systemic autoimmune disease.
The new lupus study may also help scientists start to unravel another mystery: why is the disease much more common in female patients?
“If we can establish some baseline information about the lymphoid compartment in lupus, then we can ask some of these more specific questions in the future,” says Moderbacher.