Most viruses treat the human body as a battleground. These pathogens try to infect our cells while dodging antibodies and immune cell attacks.
Herpesviruses use the human body as a cozy new home. These pathogens are experts at evading immune cells and establishing lifelong infections.
Common herpesviruses include herpes simplex virus, varicella-zoster virus (which causes chicken pox and shingles), cytomegalovirus (the number one cause of congenital birth defects), and Epstein-Barr virus (which causes mononucleosis and is linked to multiple sclerosis and certain cancers).
These are devastating viruses—and they pose a global health threat. In a 2024 report, the World Health Organization (WHO) listed herpesviruses among the top pathogens for research “prioritization” in preparation for the next pandemic.
The “silent killers”
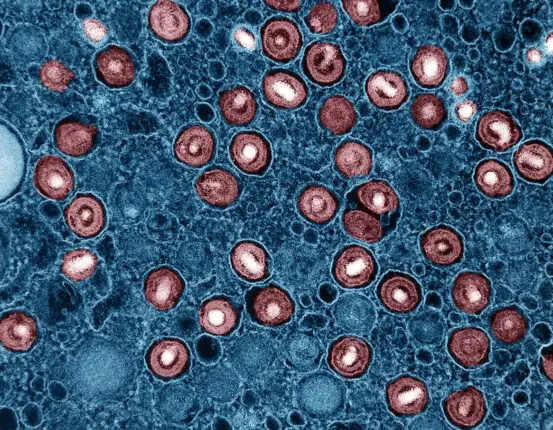
Cytomegalovirus (CMV) is an example of a herpesvirus that does more damage than most people realize. This virus passes easily through bodily fluids, such as saliva and breast milk, and infections are very common in young children and daycare workers. For most people, CMV may cause a fever and flu-like symptoms. But the story is different when a person is infected during pregnancy.
LJI Professor, President & CEO Erica Ollmann Saphire, Ph.D., MBA, calls CMV a “silent killer.” “When people get infected while they’re pregnant, their babies can be born with devastating birth defects, developmental delays, deafness, and conditions such as microcephaly,” says Saphire. “CMV-related birth defects are a $4 billion annual cost to the United States economy alone.”
A CMV vaccine would change the world. Unfortunately, many herpesviruses have proven very, very hard to beat. As LJI Professor Chris Benedict, Ph.D., explains, herpesviruses have more genes than your average virus—and they deploy these genes to trick the immune system.
“CMV and other members of the herpesvirus family have a lot of tricks up their sleeve,” says Benedict. “CMV dedicates more than half of its large genome to throw up a smokescreen for the immune system.”
For example, the Benedict Lab has discovered that the CMV genome actually allows the virus to produce a TNF-receptor-like molecule. This molecule mimics a molecule that human immune cells use to alert each other to danger. Like some kind of identity thief, CMV uses its knock-off TNF-receptor-like molecule to manipulate the immune system and escape detection.
“Here’s a virus that has been evolving with us and took some of our immune system genes as its own, molding and shaping them to establish a détente with the immune system,” says Benedict. “As a result it can hang around and never gets cleared.”
LJI scientists lead vaccine efforts
Developing herpesvirus vaccines is especially tough because these viruses can use several different protein complexes to infect host cells. “The virus has lots of different molecules on its surface that it uses to break into your cells,” says Saphire. “SARS-CoV-2, for example, has just one surface molecule that it uses to infect host cells—the target was always clear.”
But herpesviruses are very different. “These viruses have ten different complexes on the surface, so if you involve one in a vaccine, the virus doesn’t care,” Saphire says. “It’s just going to use a different complex.”
Still, herpesviruses are not invincible. LJI scientists have uncovered potential strategies to boost the body’s defenses. In fact, Benedict’s lab recently found that a subset of CD4+ “helper” T cells may help a person fight CMV and reduce the chances of the virus spreading from person to person. [Read: How ‘late-rising’ T cells combat a stubborn virus]
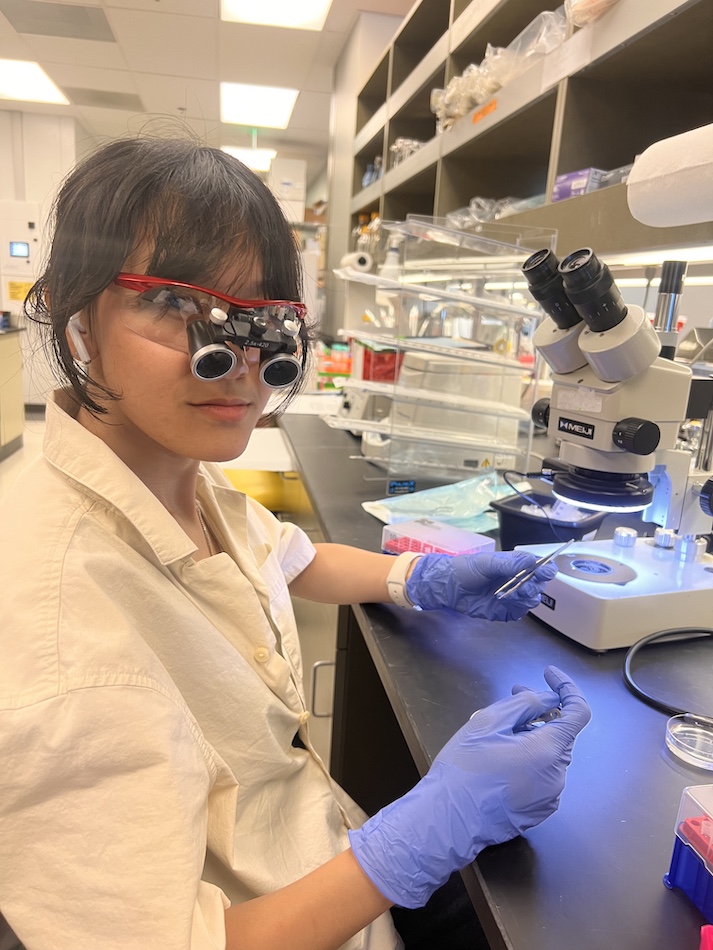
This important work recently received significant support from the U.S. government’s Advanced Research Projects Agency for Health (ARPA-H), which has granted up to $49 million toward LJI-led efforts to develop a herpesvirus vaccine. This research effort, dubbed America’s SHIELD (Strategic Herpesvirus Immune Evasion and Latency Defense), is led by LJI Professor, President & CEO Erica Ollmann Saphire, Ph.D., MBA, and includes Benedict, as well as LJI Professor Shane Crotty, Ph.D., LJI Professor Alessandro Sette, Dr.Biol.Sci., and other colleagues in LJI’s Center for Vaccine Innovation and collaborating institutions.
Over the next few years, LJI scientists and collaborators will work to develop a vaccine that provides lifelong immunity against a range of herpesviruses. As Saphire explains, it’s time to harness new tools and technologies to finally defeat these devastating pathogens.
“LJI has the most powerful microscopes commercially available, and we can get detailed images of herpesvirus proteins to understand exactly how your immune system should target these viruses,” she says. “We can profile the blood of thousands of healthy people and sick people to understand when an immune response has been effective or not and exactly why. Then we can go back and steer that vaccine to give the right kind of response.”
Herpesviruses have lurked for too long. LJI scientists want to force them into battle—a battle the human body can win.
Learn More:
LJI launches “America’s SHIELD” to develop life-saving herpesvirus vaccines