It was a case of immune cell serendipity. Greet Verstichel, M.D., Ph.D., was trying to make cancer-fighting T cells. Instead, she accidentally made the kind of T cells that respond to threats in the intestines.
These T cells had followed their own path, and Verstichel wanted to know why. At the time, Verstichel was a graduate student at Ghent University, in Belgium. As she finished her Ph.D. research, she just couldn’t stop thinking about this T cell mystery.
“There was something going on when the T cells were developing that was programming them for a certain functional ‘fate,’” Verstichel says. “There are things going on early in development that seem to have a big influence on what kind of T cell a stem cell may become. We needed to look at that process.”
T cells need a T cell receptor (TCR), a protein on the outside of a T cell. Nearly every T cell has a different TCR, which means each T cell has a different job. Some T cells specialize in attacking certain markers on cancer cells. Other T cells target cells infected by viruses such as SARS-CoV-2.
For a long time, many scientists thought T cells marched through the stages of maturation together and only learned their “fate” near the end, when they made it to the TCR stage. Yet Verstichel’s findings as a graduate student suggested something important was happening to determine T cell fate much earlier.
This puzzle led Verstichel to join the lab of LJI Professor Hilde Cheroutre, Ph.D. “I needed to think out of the box, and if there’s anyone who’s really good at that, it’s Hilde,” Verstichel says.
Where do “bad” T cells come from?
For the last five years, Verstichel has investigated what happens at the “pre-TCR stage” of T cell development. Verstichel’s recent studies show that T cells indeed develop their unique fates very early, likely during the pre-TCR stage. Her work could have a big impact on how we address autoimmune diseases.
Until recently, T cells with the TCRs to recognize healthy cells were seen as immune system mistakes. These “self-reactive” T cells are the very cells that attack organs and trigger autoimmune diseases such as type 1 diabetes.
But as scientists have used new sequencing tools to get a closer look at TCRs, they’ve realized that everyone, healthy or not, is home to an army of self-reactive T cells. “In the last decade, it’s become clear that we have both good and bad self-reactive T cells,” says Verstichel.
Some self-reactive T cells protect the body, but some are potentially harmful. “Where are decisions made to either keep a T cell around or eliminate it?” says Verstichel. “Or in the case of a person with autoimmune disease—why does the body fail to eliminate those self-reactive T cells?”
Verstichel wondered if self-reactive T cells are directed by more than their TCR. Perhaps other genes are at play to “aim” a T cell at its target.
To find out, she worked closely with Ichiro Taniuchi, Ph.D., and Kiyokazu Kakugawa, Ph.D., of the RIKEN Research Center for Allergy and Immunology. The team developed a mouse model to study a gene that normally protects against autoimmune diabetes in mice. Thanks to this gene, mice normally take about 100 days to develop the disease. When the researchers added a pre-TCR mutation to this gene in T cells in a mouse model, the mice developed diabetes very quickly.
The pre-TCR mutation Verstichel studied is a useful example of how small changes in gene expression early on can determine T cell fate.
What about human cells?
In 2020, Verstichel’s research got a boost in funding from The Tullie and Rickey Families SPARK Awards for Innovations in Immunology, an LJI program that supports high-risk, high-reward projects led by early career scientists. Her project was supported by donors Barbara Donnell, Maria Silva, Bill Passey, and several others.
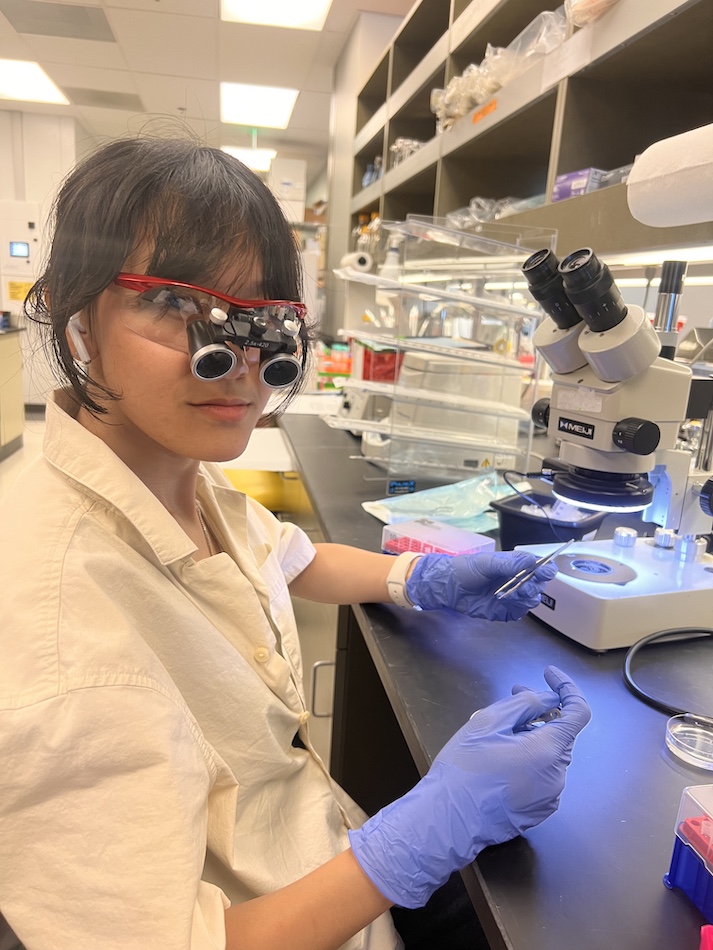
Verstichel’s Tullie and Rickey Families SPARK Award allowed her to examine gene expression and T cell fate in human cells. Because Verstichel couldn’t manipulate actual human development, she devised a cell culture model using thymus tissue. Looking at the thymus is critical because this is the organ where T cells mature (and where they get the “T” in their name).
Thymus tissues in her research come from donated samples collected at Rady Children’s Hospital. “Surgeons have to cut away some of the thymus tissue to do heart operation in children, and they used to just toss the tissue,” says Verstichel. “Now, thanks to this collaboration, they are sending that tissue to LJI so we can study it.”
Verstichel isolated stem cells from the thymus tissue and tracked how they develop. She then sequenced the genes in these mature T cells to understand exactly what they are doing in the body. She also inhibited certain genes to see how small changes affect T cell fate.
She’s now confirmed that the phenomenon she discovered in mice holds true in humans. Whether a self-reactive T cell is good or bad is determined through gene expression changes very early on. Verstichel hopes scientists can use these findings to better manipulate T cells and prevent disease.
Verstichel’s work has caught the attention of the Praespero Foundation, which awarded the team a $400,000 grant to continue with the investigation. “I’ve been very fortunate to get to work on this full time at LJI—that the foundation and Hilde believed in this project enough to keep it going,” says Verstichel.
Earlier this Spring, Verstichel presented her findings in an LJI seminar, giving her colleagues an in-depth look at a critical process in T cells. After the presentation, researchers from across the Institute came up to Verstichel. They had been in the same position she found herself in as a graduate student back in Belgium. Unexpected T cells were showing up in their studies, and they weren’t sure why these cells looked different from the others.
“People were coming up after that talk saying, ‘Yeah! We see these T cells too!’” says Verstichel.
Verstichel had finally opened the door to finding answers—and harnessing T cells to better combat disease.