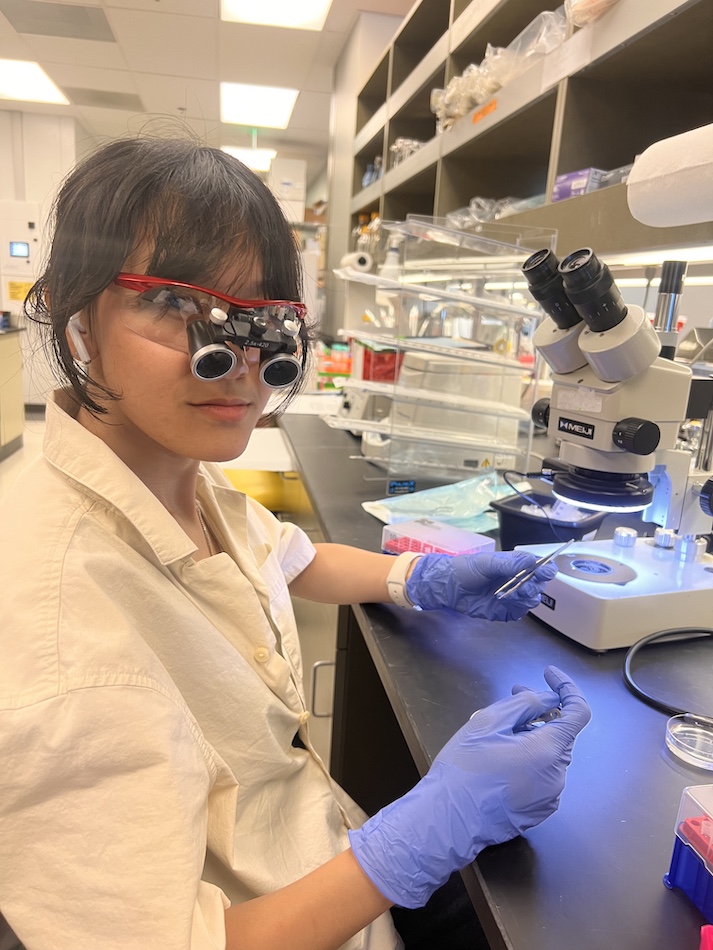
Julia Timis just can’t avoid mosquitos. She’s one of those people who ends up with a dozen bites on a summer evening. “When you’re with me, you will be safe from mosquitoes, because they always find me,” says Timis, who works as a technician in the laboratory of Professor Sujan Shresta, Ph.D., at La Jolla Institute for Immunology (LJI).
Fortunately, Timis has the privilege of living and working in San Diego, where mosquito-borne viruses are extremely rare. Just three people in the sprawling county were diagnosed with West Nile virus in 2021. Dengue virus, yellow fever virus, and Zika virus aren’t endemic here—yet.
Thanks to climate change, the Aedes mosquitoes that carry these viruses are moving into new regions. Countries like Nepal, which never used to have dengue cases, now see thousands of cases a year.
“Almost 4 billion people, so half of the world’s population, is at risk of infection with one of these viruses,” says Timis. “Dengue alone infects 390 million people annually, and infants and young children are especially vulnerable to developing severe dengue infections. We really need a vaccine against these diseases.”
As a member of the Shresta Lab, Timis is working to guide vaccine design by shedding light on the human immune response to flaviviruses, the viral family that includes dengue virus, Zika virus, yellow fever virus, and Japanese encephalitis virus (JEV).
Timis is originally from Austria, and she found her passion for science early on. She was always interested in the invisible side of biology—the microscopic battles between pathogens and the immune system. “We can’t see our immune cells, but just being sick and knowing what kind of cells are fighting in your body and helping you get better is just really awesome,” says Timis.
As she completed her master’s degree, she was lucky enough to spend time interning in a flavivirus research laboratory in Thailand. There she learned about day-to-day life in a country where mosquito bites can be devastating. “People who live there can’t be covered in mosquito repellent 24/7. There is always going to be the risk of getting infected,” says Timis. “That was eye-opening for me.”
As we spoke for this article, Timis had another virus in mind: SARS-CoV-2. She was home with a case of COVID-19, and she tried not to cough on the phone. After more than two years of the pandemic, catching the virus had come to feel inevitable, she said.
Timis sees a lot of parallels between flaviruses and coronaviruses. For one thing, both types of pathogens can spread undetected. Many people with dengue virus, for example, don’t show symptoms. Mosquitoes then suck their blood and can potentially pass the virus to a more vulnerable person. Both families of viruses also have the potential to emerge in new places, infecting people with no pre-existing immune protection.
We have life-saving vaccines for COVID-19 now, but no good options yet against flaviviruses.
Timis’ work with Shresta and other LJI scientists may help change that. Because flaviviruses overlap in many places, they’ve set out to test a “pan-flavivirus” vaccine that can neutralize several viruses at once. Timis works with mouse models, developed by the Shresta Lab, to investigate the role of T-cell immunity in animals vaccinated with an experimental pan-flavivirus RNA vaccine.
This potential vaccine targets a specific site, or “epitope,” that is the same on several dengue virus variants, as well as Zika. The hope is that an activated T cell population will help neutralize these viruses.
Timis’ research with mouse models is especially useful for testing whether this experimental vaccine avoids a phenomenon called antibody-dependent enhancement (ADE), where immunity against one flavivirus can actually enhance the severity of a subsequent infection with a flavivirus of a different serotype (such as a dengue type with different features). The team hopes that by engaging T cells to fight flaviviruses, they won’t trigger a negative antibody response.
She hopes that witnessing the COVID-19 pandemic has helped more people understand the urgency of flavivirus vaccine research.
“We’ve seen a big community of lay people getting more interested in the field and wanting to understand more basic principles in immunology,” says Timis. “If everyone wants to learn a little, I think it’s going to help.”