Japanese Encephalitis
Japanese encephalitis is a viral disease transmitted primarily by mosquitos. The disease can cause inflammation of the brain, and is the most common cause of encephalitis in many Asian countries.
The disease is caused by Japanese encephalitis virus (JEV), a species if flavivirus closely related to dengue virus, Zika virus, and West Nile virus, and yellow fever virus.
There is no cure for Japanese encephalitis, but safe and effective vaccines are available to protect against severe disease.
Our Approach
Scientists at La Jolla Institute for Immunology (LJI) are working to shape an effective vaccine strategy that addresses JEV along with other flaviviruses.
LJI Professor Sujan Shresta, Ph.D., and her team are investigating what happens when a person encounters more than one flavivirus. In response to flavivirus infection or vaccination, the immune system trains antibodies to recognize viral particles. Dr. Shresta has found that antibodies trained to recognize JEV are prone to later allowing Zika virus to enter cells, resulting in a more severe Zika infection. This phenomenon is called antibody-dependent enhancement (ADE).
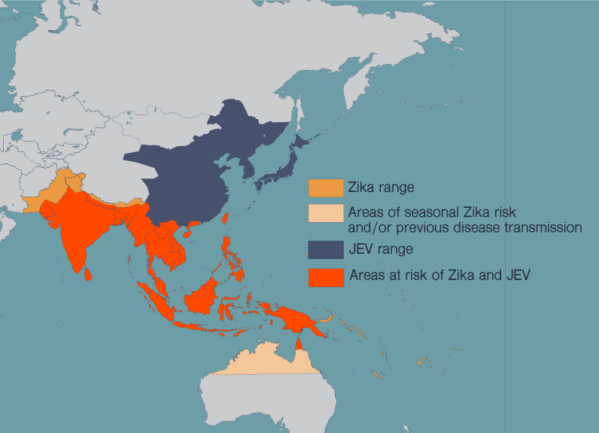
Researchers need to address this example of ADE as they design vaccines that can be deployed in regions where JEV and Zika are both present. Dr. Shresta has shown that vaccines that prompt a strong T cell response from the immune system can counteract the effects of harmful antibodies in ADE.
In 2024, Dr. Shresta received substantial funding through the National Institute for Allergy and Infectious Diseases’ (NIAID) Flavivirus and Alphavirus ReVAMPP (FLARE) program to test experimental vaccine strategies against deadly viruses from the flavivirus and alphavirus families, including dengue virus and chikungunya. The goal is for research with dengue virus vaccines will help Dr. Shresta and her colleagues develop effective JEV vaccines as well.
LJI is also home to the Immune Epitope Database (IEDB), led by LJI Professors Alessandro Sette, Dr. Biol. Sci., and Bjoern Peters, Ph.D. Scientists worldwide can use this free online resource to learn more about how the immune system reacts to JEV and many other pathogens. By understanding the immune system targets sites, or epitopes, on the virus, researchers can design more precise vaccines and therapies.
This JEV research is part of LJI’s work toward pandemic preparedness. Along with Dr. Sette, LJI Research Assistant Professor Alba Grifoni is investigating mosquito-borne viruses such as JEV as part of a CEPI-funded effort to boost pandemic preparedness.
Learn more:
Related News
- Institute News
- Research News