Lung Cancer
Lung cancer is the leading cause of cancer death for both men and women in the United States, according to the American Cancer Society.
Lung cancers usually fall into two categories: small cell and non-small cell. Small cell lung cancer is a faster-growing form of the disease. According to the American Cancer Society, SCLC tends to respond well to chemotherapy and radiation, but the cancer will return for most people. Non-small cell lung cancer (NSCLC) is more common but tends to grow more slowly than SCLC. Types of NSCLC include adenocarcinoma and squamous cell carcinoma.
Lung cancer tends to affect people over the age of 60. Smoking is the biggest risk factor—and it contributes to 80 percent and 90 percent of lung cancer deaths in women and men, respectively. According to a U.S. Surgeon General report, second-hand smoke leads to approximately 7,330 lung cancer deaths among nonsmokers every year.
Lung cancer is often deadly because tumors are not caught early enough. Once tumors are diagnosed, they are often inoperable or have already metastasized. Better diagnostics and more effective therapies are desperately needed in the field.
Our Approach
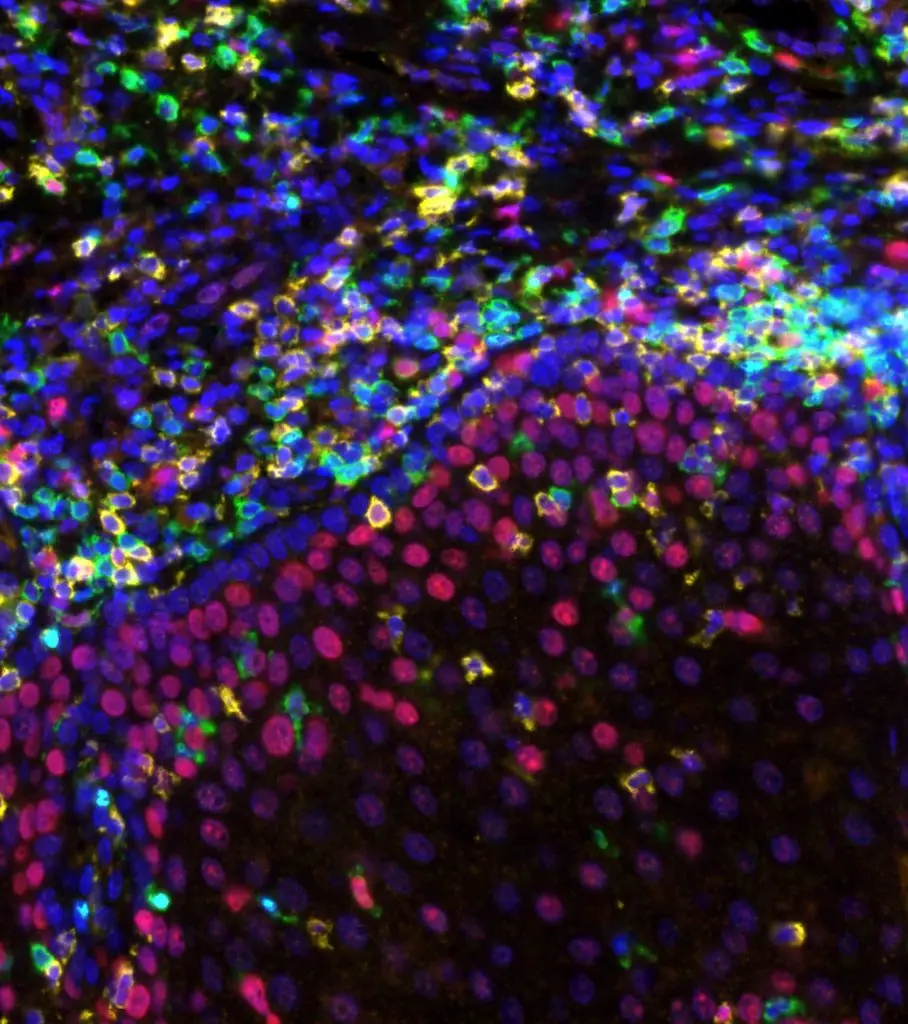
Researchers at La Jolla Institute for Immunology (LJI) are studying ways to harness the immune system to halt lung cancer growth.
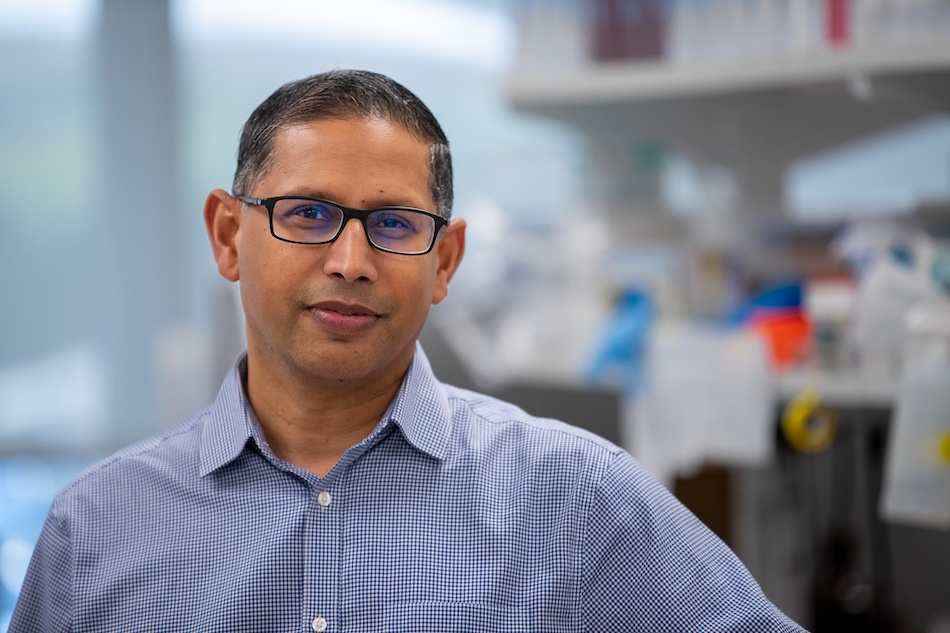
LJI Professor Pandurangan Vijayanand, M.D., Ph.D., is investigating how immunotherapies could take aim at lung cancer. In a 2017 Nature study, his lab showed that certain anti-tumor cells called cytotoxic T lymphocytes (CTLs) have molecular features associated with a robust anti-tumor immune response. This study defined the “molecular fingerprint” of tumor-infiltrating CTLs and identified potentially new targets for immunotherapy.
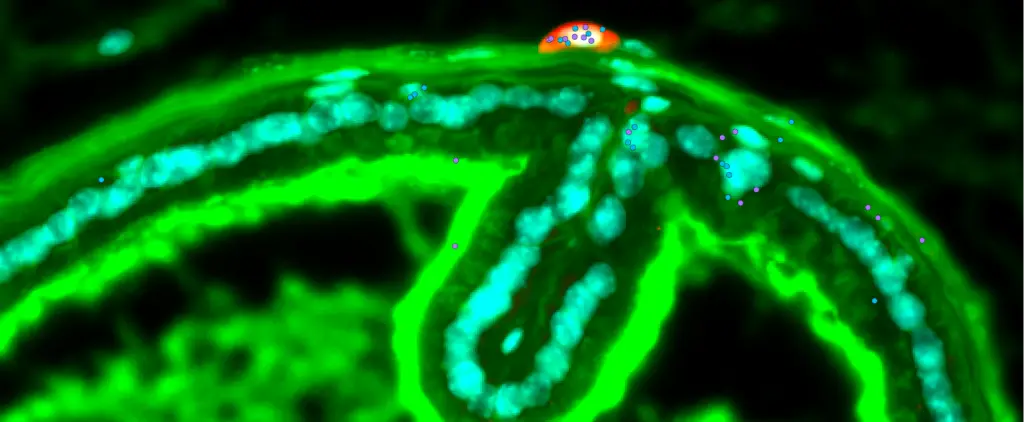
LJI Assistant Professor Miguel Reina-Campos is investigating the cancer-fighting power of specialized immune cells called tissue-resident T cells. These T cells have adapted to living in specific organs, such as the lungs, and are well suited to killing solid tumors that may try to develop in those organs. Dr. Reina-Campus aims to investigate the basis of this T cell immunity to improve life-saving cancer immunotherapies.
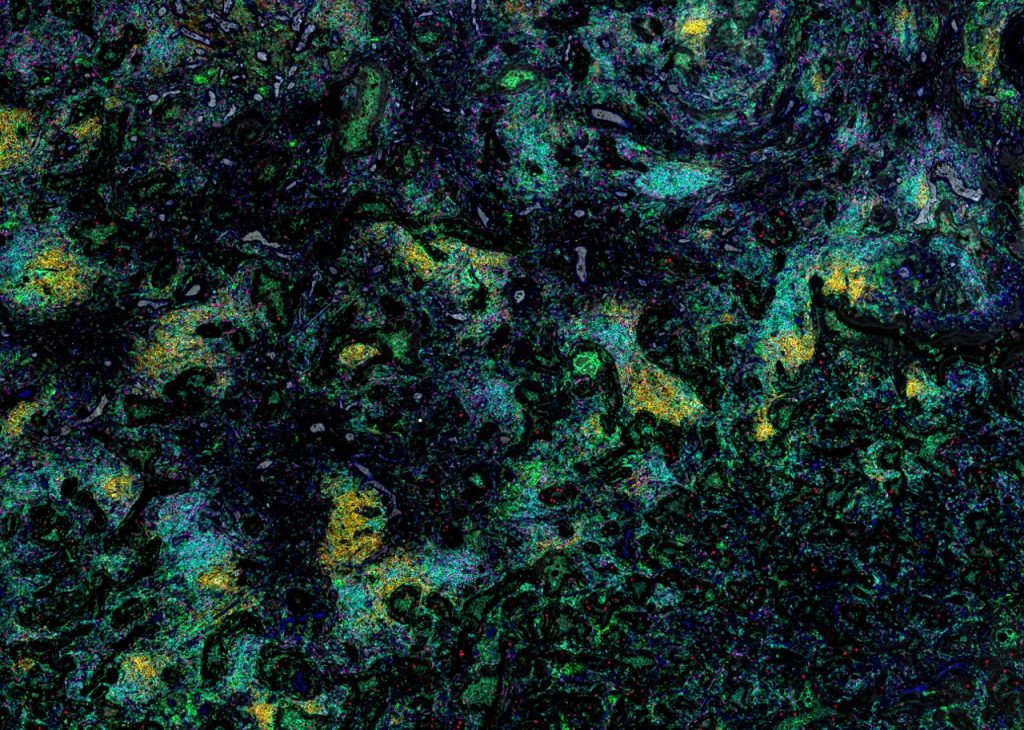
In a 2024 study, LJI Professor Stephen Schoenberger, Ph.D. and LJI Professor Bjoern Peters, Ph.D., found that many patients thought to have immunologically “cold” tumors (which didn’t spark a strong reaction from immune system defenses) actually do make cancer-fighting T cells. This was true for many types of cancers, including lung cancers. This research opens to door to potentially harnessing this pre-existing natural immunity to boost the immune system’s ability to fight these tumors.
Learn more:
Related News
- Research News
- Institute News
- Research News