Measles
Measles is a highly contagious disease caused by an airborne virus called rubeola virus (not to be confused with rubella or “German measles”). This virus spreads from person to person when an infected person coughs, sneezes, or breathes. Patients with measles may experience a high fever, cough, runny nose, and a painful, full-body rash. The disease can be fatal, especially in infants and children.
Most people in the United States are vaccinated against measles, mumps, and rubella (MMR) during childhood. Many teens and adults are encouraged to stay up to date on their MMR vaccine, especially if they work in a healthcare setting, work with children, or may bear children. [See CDC Vaccination Information]
Despite the safety and effectiveness of the MMR vaccine, many people still die of measles worldwide. In 2021, more than 136,000 people died from measles, according to the World Health Organization (WHO).
As WHO and other organizations try to vaccinate more people across the globe, many scientists are working to improve vaccines and therapies against rubeola virus. This work is important for future pandemic preparedness.
Researchers have identified paramyxoviruses as a viral family with a high pandemic potential. Rubeola virus is a member of the Paramyxovirus family, which includes the deadly Nipah virus and 73 other related viruses. The risk of a deadly, highly contagious paramyxovirus emerging has led The Coalition for Epidemic Preparedness Innovation (CEPI) to call paramyxoviruses one of “The Viral Most Wanted.”
Our Approach
Scientists at La Jolla Institute for Immunology (LJI) are working to improve vaccines and therapies against measles and related paramyxoviruses.
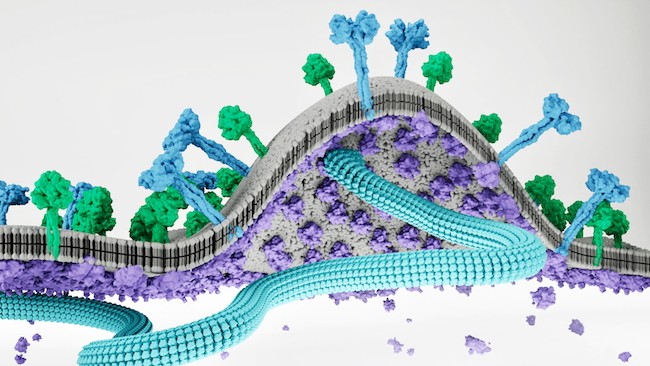
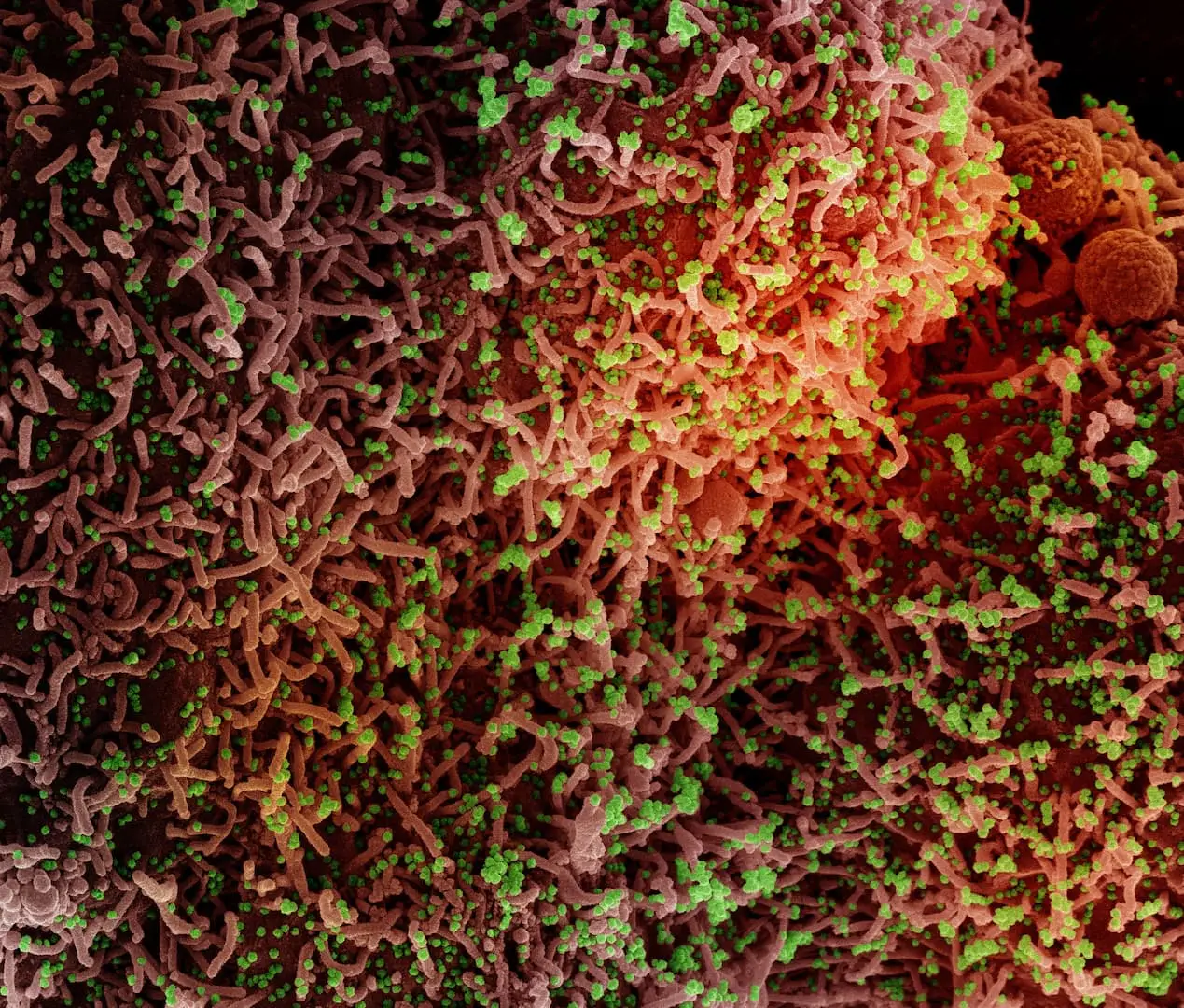
LJI Professor, President, and CEO Erica Ollmann Saphire, Ph.D., is studying how rubeola virus makes copies of itself inside infected host cells. Her lab has discovered how a related virus, called Nipah virus, uses several key proteins to assemble its viral proteins and “bud” off from a host cell and further spread the infection through a host. Dr. Saphire’s findings suggest these proteins play the same important roles in rubeola virus infection.
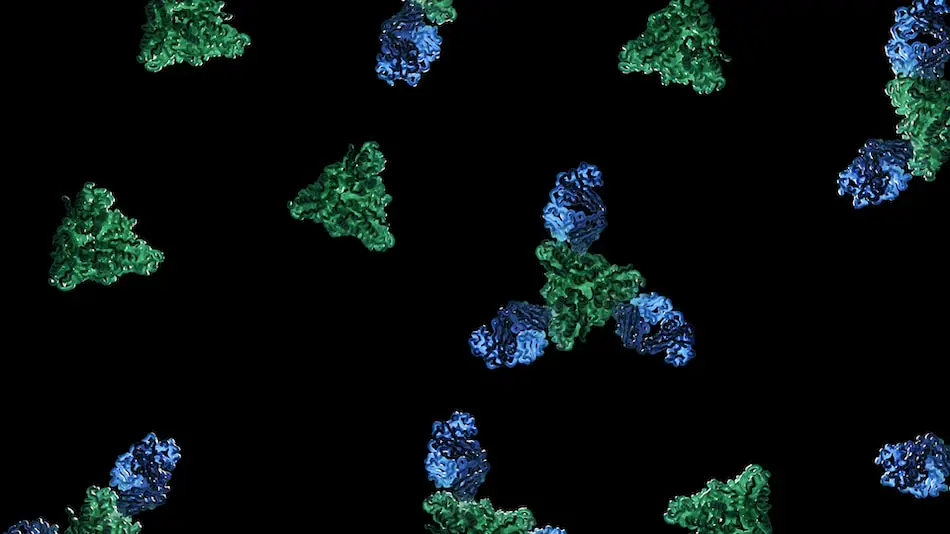
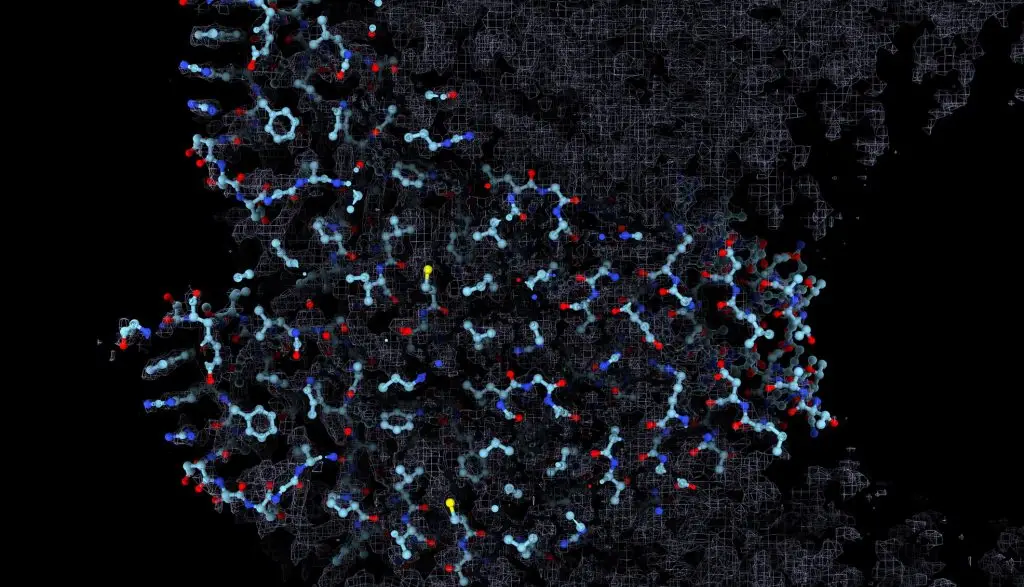
LJI scientists are also investigating the the measles virus fusion process, which allows the virus to fuse with a host cell and initiate infection. In a 2024 Science study, scientists in the Saphire Lab harnessed an imaging technique called cryo-electron microscopy to show—in unprecedented detail—how a powerful antibody can neutralize the virus before it completes the fusion process.
Scientists can use these valuable insights when designing new measles vaccines and therapeutics that halt infection by interrupting the viral life cycle.
Dr. Saphire’s lab is also working to help the scientific community respond more quickly to any future viral pandemic, including a paramyxovirus-related pandemic, by advancing the use of high-resolution imaging technologies. The researchers recently received funding through the Department of Energy’s Biopreparedness Research Virtual Environment (BRaVE) initiative to help accelerate a method called x-ray crystallography, which scientists can use to capture detailed, 3D images of how antibodies target rubeola and other viruses.
LJI Professor Alessandro Sette, Dr.Biol.Sci., and LJI Research Assistant Professor Alba Grifoni, Ph.D., are investigating how T cells recognize and fight paramyxovirus infections. They’ve received funding from CEPI to study the sites, called epitopes, where these viruses are vulnerable to a host’s T cell response.
One valuable tool for this paramyxovirus research is the LJI-hosted Immune Epitope Database (IEDB) which houses T cell data from measles researchers around the world. The IEDB gives scientists a window into how the immune system can target measles and other paramyxoviruses. The IEDB also lets scientists compare T cell responses between species of paramyxoviruses, which is extremely helpful for predicting how the immune system might respond to a future paramyxovirus with pandemic potential.
Learn more:
Related News
- Research News
- Immune Matters
- Research News