Our Approach
Scientists at La Jolla Institute for Immunology (LJI) direct cutting-edge research into how the body’s immune cells recognize and fight S. pneumoniae infection.
LJI Professor Mitchell Kronenberg, Ph.D., leads efforts to understand how healthy individuals contain infection by bacteria such S. pneumoniae. His team focuses on specialized populations of immune cells that make very rapid or innate-like immune responses against the pathogen. They have found that when S. pneumoniae invades the lung, immune cells called invariant natural killer T (iNKT) cells mount an immediate and highly choreographed immune response that prevents the infection from progressing. Moreover, since iNKT cells in different patients appear to target S. pneumoniae in the same way (unlike other types of T cells), scientists hope to find ways to activate these cells to fight pneumonia in newly infected patients.
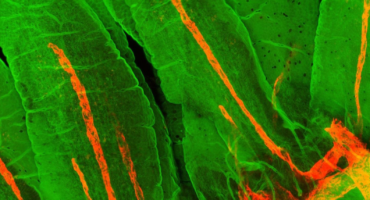
Dr. Kronenberg’s team is using mouse models and cutting-edge intravital microscopy to follow iNKT cell mobilization in living animals after S. pneumoniae infection. Their research charts how different subsets of iNKT cells emerge following infection, each secreting different chemical messenger (cytokine) signals at the “right” time. Thanks to this research, we now know that iNKT cell subsets can only neutralize lung infections if they are activated in a certain order in the right part of the airway. Researchers can build upon these findings to design potent pneumonia vaccines.
LJI Professor Bjoern Peters, Ph.D., recently received NIH funding to investigate how the immune system’s T cells recognize and target vulnerable sites, or “epitopes,” on S. pneumoniae. For this project, Dr. Peters and his team are developing a bioinformatics approach identify peptide candidates that are then synthesized and screened for recognition by T cells—which will help reveal T cell epitopes. The Peters lab is also working with patient cohorts to uncover T cells epitopes identified from these large-scale screens for their HLA restriction, their ability to bind different HLA molecules, and their recognition in different patient cohorts.
Learn more: