Our Approach
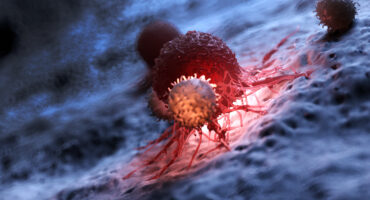
Scientists at La Jolla Institute for Immunology (LJI) are investigating what causes immune cells to turn on the body—and how we can intervene.
What triggers autoimmune diseases
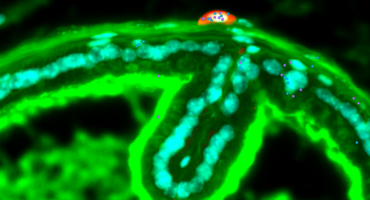
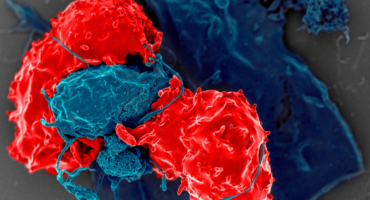
LJI Professor Hilde Cheroutre, Ph.D., is studying how autoreactive T cells mistakenly learn to recognize “self” in an organ called the thymus. These “educated” autoreactive T cells can actually help the body by regulating immune responses to cancer cells or infected cells. But under the wrong circumstances, a naïve T cell may encounter a self-antigen and spark an autoimmune response. Dr. Cheroutre and her team are working with doctors at Rady Children’s Hospital-San Diego to better understand how this process goes wrong. The team hopes to be able to identify the signs that an infant might be susceptible to autoimmune diseases and perhaps even prevent autoimmunity altogether.
LJI scientists have also received significant support from the Global Autoimmune Institute (GAI) to investigate the beginnings of autoimmune disease processes. In 2024, GAI granted funding to LJI faculty member Sam Myers, Ph.D., who now serves as LJI’s Global Autoimmune Institute Assistant Professor. The GAI funding also supported ongoing research by LJI Postdoctoral Researcher Greet Verstichel, M.D., Ph.D., into autoimmune disease mechanisms.
A closer look at specific autoimmune diseases
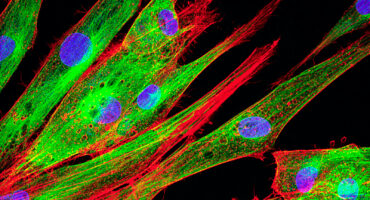
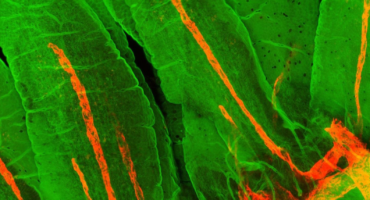
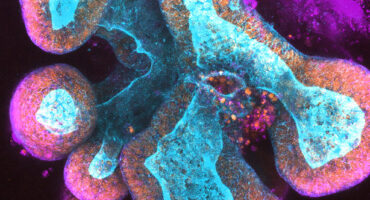
LJI Associate Professor Sonia Sharma, Ph.D., is studying inflammatory and autoimmune diseases that affect the vascular endothelium, the cells lining the blood vessels. Her laboratory integrates cutting-edge genetics, biochemistry, cell biology, computational and translational approaches to define the key genetic mechanisms regulating cellular innate immunity—and determine how these factors can trigger autoimmune disease.
LJI Professor Michael Croft, Ph.D., studies molecules involved in causing atopic dermatitis, severe asthma and fibrotic diseases caused by chronic inflammation. He has partnered successfully with several companies and his work has led to clinical trials for asthma and atopic dermatitis.
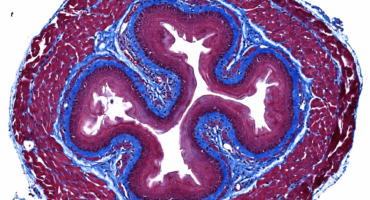
LJI Professor Mitchell Kronenberg, Ph.D., is investigating how surface molecules and intracellular signaling pathways regulate immune cells that reside in the intestine. These immune cells have a unique challenge because they must co-exist with a highly diverse microbiome. He studies how these cells maintain this peaceful co-existence while responding to pathogens. The loss of tolerance of good bacteria is a key step involved in the pathogenesis of inflammatory bowel diseases (IBD), such as Crohn’s disease and ulcerative colitis.
Dr. Sette has also teamed up with LJI Professor Bjoern Peters, Ph.D., to build the Immune Epitope Database (IEDB), a publicly available online resource that includes data from researchers around the world. The IEDB is a valuable tool for studying the chemical aspects of what immune cells recognize when they make an immune response, including when they mistakenly target a person’s own organs in different autoimmune diseases.
Autoimmunity and age-related diseases
The lab of LJI Professor Alessandro Sette, Dr. Biol. Sci., is investigating autoimmune diseases from two angles. First, the team is looking at the possible role of autoreactive T cells in causing Parkinson’s disease. Dr. Sette and collaborator LJI Adjunct Professor, have found that T cells can target misfolded clumps of alpha-synuclein protein in the brain, potentially triggering damage to vulnerable brain cells very early in the disease onset. This research could make it possible to someday detect Parkinson’s disease before the onset of debilitating motor symptoms—and potentially intervene with therapies to slow the disease progression.
Sex-based differences in autoimmune disease
Dr. Sharma and many researchers in LJI’s Center for Sex-Based Differences in the Immune System are working to understand why many autoimmune diseases affect men and women differently.
LJI Professor Pandurangan Vijayanand, M.D. Ph.D., and LJI Research Assistant Professor Benjamin J. Schmiedel, Ph.D., are studying genomic data from patients to see which commonly found genetic variants are more prevalent in people with different autoimmune diseases. Dr. Vijayanand and his LJI colleagues have built a database called DICE (Database of Immune Cell Expression, Expression of quantitative trait loci, and Epigenomics), which scientists can use to study the effects of different genetic variants in different immune cells.
In 2018, the team published data from 91 healthy donors showing profiles of genetic activity for the 15 most abundant types of immune cells found in human blood. Because autoimmune diseases usually arise from combinations of variants in many different genes, some of which are common and also found in individuals without autoimmune disease, the database gives scientists a guide for comparing variants more often associated with health compared to disease-associated variants. In 2022, Vijayanand’s team reported the discovery of new subsets of CD4+ ‘helper’ T cells linked to autoimmunity and that appear to vary in men and women.
Learn more:
LJI Center for Autoimmunity and Inflammation