Flashback to mid-March: the novel coronavirus had reached San Diego, California. Few people could get tested, and even less was known about how the virus mutated as it spread from person to person.
Scientists now know that two variants of the novel coronavirus (SARS-CoV-2) were circulating at that time. The variants, called G614 and D614, had just a small difference in their “spike” protein—the viral machinery that coronaviruses use to enter host cells.
In a new study, an international team of scientists show that the G version of the virus has come to dominate cases around the world. They report that this mutation does not make the virus more deadly, but it does help the virus copy itself, resulting in a higher viral load, or “titer,” in patients.
The new study, led by scientists at Duke University, Los Alamos National Laboratory and La Jolla Institute (LJI) was published July 2, 2020 in Cell.
“We are focused on the human immune response because LJI is the headquarters for the Coronavirus Immunotherapy Consortium (CoVIC), a global collaboration to understand and advance antibody treatments against the virus,” says LJI Professor Erica Ollmann Saphire, Ph.D., who leads the Gates Foundation-supported CoVIC.
Saphire explains that viruses regularly acquire mutations to help them “escape” antibodies made by the human immune system. When a virus acquires many of these individual changes, it “drifts” away from the original virus. Researchers call this phenomenon “antigenic drift.” Antigenic drift is part of the reason you need a new flu shot each year.
It is extremely important for researchers to track antigenic drift as they design vaccines and therapeutics for COVID-19.
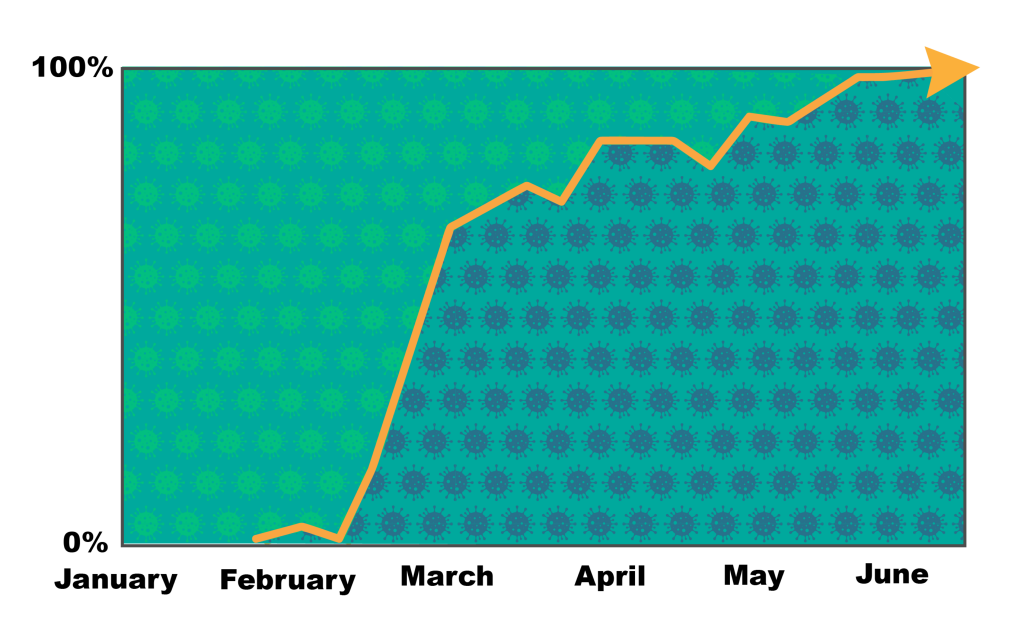
For the study, Saphire collaborated with Bette Korber, Ph.D., a fellow at Los Alamos National Laboratory (LANL), who serves as senior author of the study. Korber and her colleagues at LANL have developed tools to track mutations around the world. In the new study, their tracking showed that while the G and D viruses both spread widely around the world, the G virus was “fixed” as the dominant variant by mid-March.
Meanwhile, Saphire and co-author David Montefiore, Ph.D., of Duke University Medical Center, led research into the immune response to these variants. They determined that viruses carrying spike with the G mutation grew two to three times more efficiently, leading to a higher titer. Saphire and her colleagues then used samples from six San Diego residents to test how human antibodies neutralized the D and G viruses. Would the fast-growing G virus be harder to fight?
Their experiments showed that the human immune response could neutralize the new G virus as well or better than the original D virus. This meant the immune system didn’t need to produce more antibodies or better antibodies against the G virus, even though this variant was more successful at spreading. This finding was in line with what doctors saw in COVID-19 patients.
“The clinical data in this paper from the University of Sheffield showed that even though patients with the new G virus carried more copies of the virus than patients infected with D, there wasn’t a corresponding increase in the severity of illness,” says Saphire.
Korber adds, “These findings suggest that the newer form of the virus may be even more readily transmitted than the original form—whether or not that conclusion is ultimately confirmed, it highlights the value of what were already good ideas: to wear masks and to maintain social distancing.”
Saphire says the novel coronavirus could be successful precisely because many patients do only get a mild version, or no symptoms at all.
“The virus doesn’t ‘want’ to be more lethal. It ‘wants’ to be more transmissible,” Saphire explains. “A virus ‘wants’ you to help it spread copies of itself. It ‘wants’ you to go to work and school and social gatherings and transmit it to new hosts. Of course, a virus is inanimate—it doesn’t ‘want’ anything. But a surviving virus is one that disseminates further and more efficiently. A virus that kills its host rapidly doesn’t go as far—think of cases of Ebola. A virus that lets its host go about their business will disseminate better—like with the common cold.”
So while the G mutation doesn’t make cases more severe, a different mutation might. “We’ll be keeping an eye on it,” says Saphire.
The study, titled, “Tracking changes in SARS-CoV-2 Spike: evidence that D614G increases infectivity of the COVID-19 virus” was supported by the Medical Research Council (MRC) part of UK Research & Innovation (UKRI); the National Institute of Health Research (NIHR); Genome Research Limited, operating as the Wellcome Sanger Institute; a Wellcome Trust Intermediate Clinical Fellowship (110058/Z/15/Z); CoVIC, INV-006133 of the COVID-19 Therapeutics Accelerator, supported by the Bill and Melinda Gates Foundation, Mastercard, Wellcome; private philanthropic support, as well as the Overton family; a FastGrant, from Emergent Ventures, in aid of COVID-19 research; and the National Institute of Allergy and Infectious Diseases, National Institutes of Health, Department of Health and Human Services, under Interagency Agreement No. AAI12007-001-00000.
Additional study authors included W.M. Fischer, S. Gnanakaran, H. Yoon, J. Theiler, W. Abfalterer, N. Hengartner, E.E. Giorgi, T. Bhattacharya, B. Foley, K.M. Hastie, M.D. Parker, D.G. Partridge, C.M. Evans, T.M. Freeman, T.I. de Silva, C. McDanal, L.G. Perez, H. Tang, A. Moon-Walker, S.P. Whelan and C.C. LaBranche.





