LA JOLLA, CA—Scientists at La Jolla Institute for Immunology (LJI) are investigating how the mutated “clade 1” mpox virus may affect children and older patients—and how new vaccines can help the body fight back. This research may provide important insights for vaccine and therapeutic use as health officials combat the growing mpox outbreak in the Democratic Republic of Congo and more than a dozen African countries.
The World Health Organization has declared the clade I mpox outbreak a “public health emergency of international concern,” and officials have confirmed that a patient in Sweden is being treated for this new mpox strain. The patient contracted the virus when traveling in Africa.
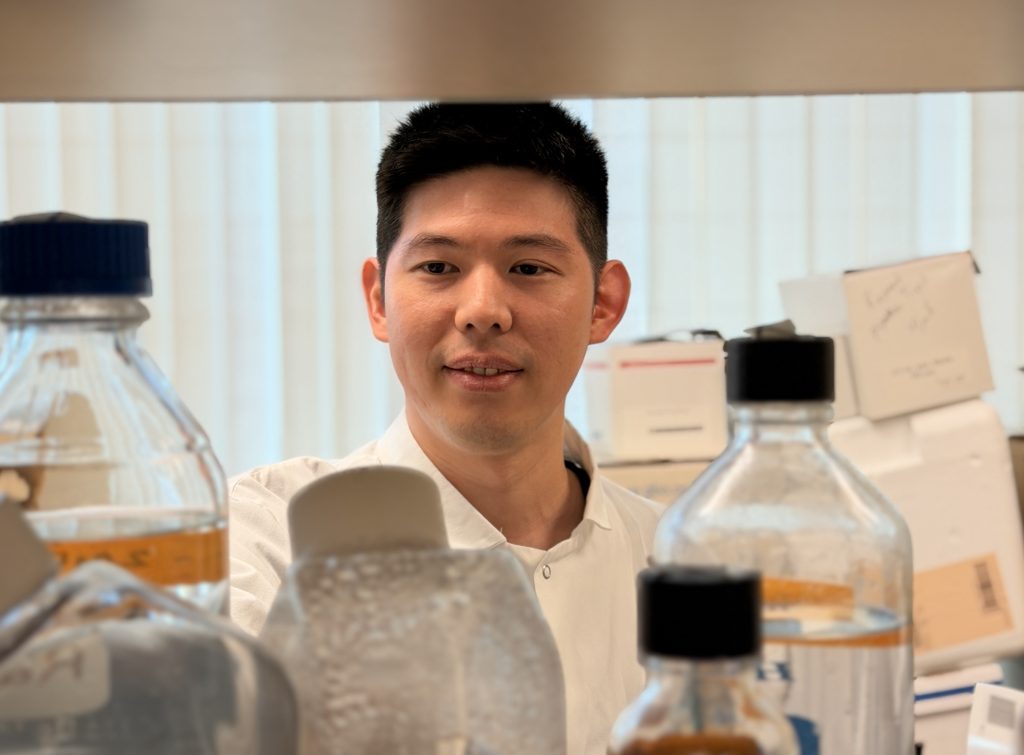
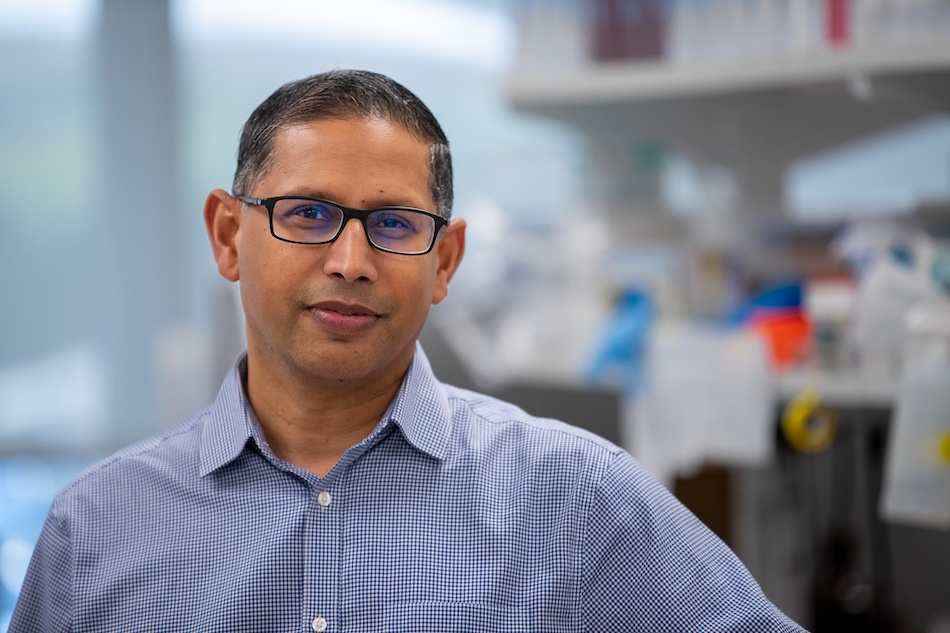
LJI Professor Alessandro Sette, Dr.Biol.Sci., and LJI Research Assistant Professor Alba Grifoni, Ph.D., are leading important work to understand how mpox-fighting T cells protect the body from severe disease.
“The new clade I mpox virus is brand new, so the situation is evolving rapidly,” says Sette, who also serves as Co-Director of the LJI Center for Vaccine Innovation.
According to the U.S. Centers for Disease Control and Prevention:
- The new outbreak is caused by a “clade I” strain of the mpox virus. The 2022 mpox outbreak came from a “clade II” mpox virus.
- TClade I mpox viruses represent a different branch of the mpox family tree. Clade I mpox viruses are known for causing more severe cases and fatalities compared to clade II.
- TThe clade I mpox virus appears to be more transmissible through skin-to-skin contact, and it has spread more widely among children under age 15.
- TThe change in susceptible population is noteworthy because the 2022 mpox outbreak was seen mostly in relatively young men having sex with men.
Sette and Grifoni hope their work can guide future mpox vaccine development and help protect a broad group of patients.
“The new viral behavior could change the game and also affect a broader range of patients, including more children, women, and older patients,” says Sette. “We will look at immune responses in different groups and see if there are age or sex-based differences.”
Building on mpox expertise
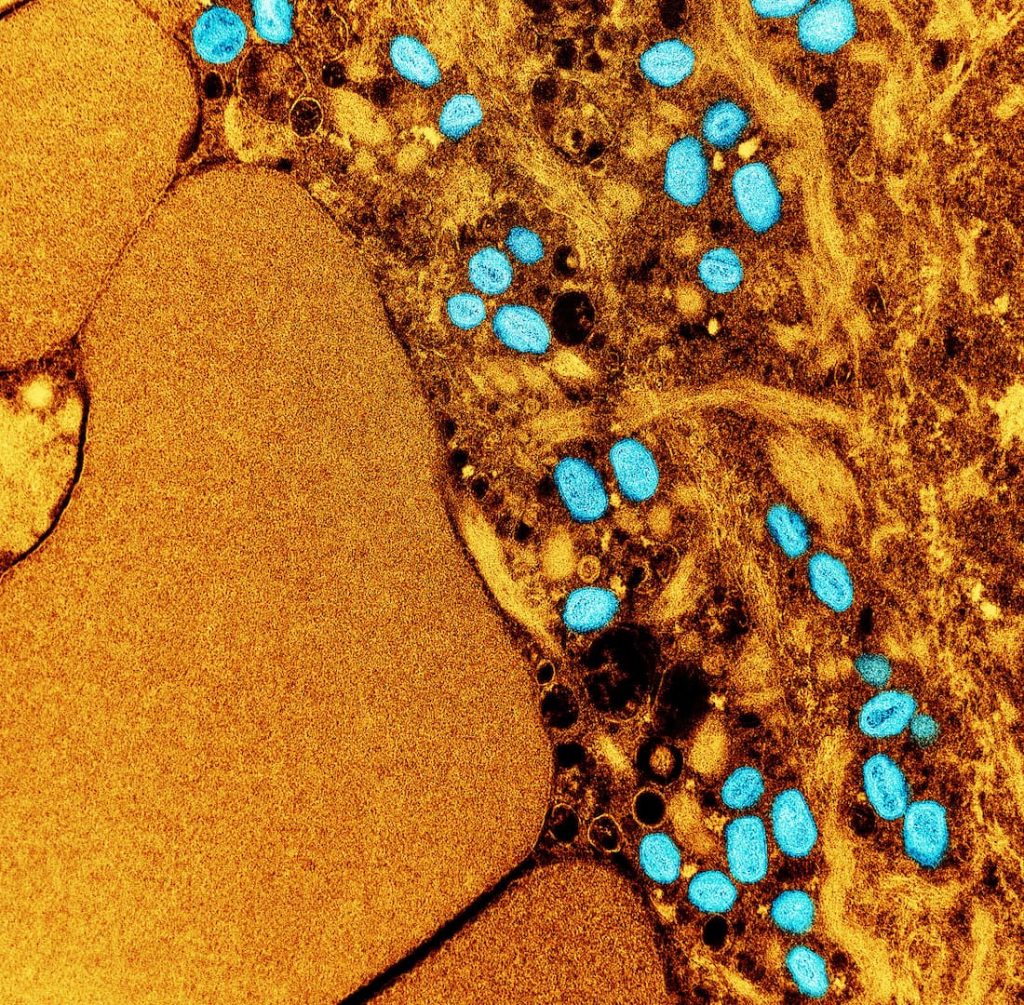
This research builds on previous LJI findings. In a 2022 Cell Host & Microbe study, Sette and Grifoni laboratories found that the current JYNNEOS and Modified Vaccinia Ankara (MVA) vaccines can train T cells to recognize vulnerable targets (called epitopes) on mpox.
In follow-up studies, Sette, Grifoni, and their LJI colleagues found that human T cells are good at recognizing many epitopes on the original mpox strain. Instead of hunting for one bulls-eye, T cells can take aim at many targets to stop mpox virus from spreading in the body.
The LJI researchers found that current mpox vaccines can help boost that T cell protection. “That research suggested that the current mpox vaccines can protect against severe disease, but these vaccines aren’t limiting the spread of infection,” says Grifoni.
LJI scientists compare mpox viruses
The question now: Can current vaccines also train T cells to recognize epitopes from the new mpox strain?
“It’s clear that this is a new strain of mpox, but it’s not clear how different this virus is from the 2022 strain—or where the differences are in the viral proteins,” says Sette.
As Sette explains, mpox is known as a large DNA virus, which means it is unlikely to mutate in many areas that include T cell epitopes. Other viruses, such as SARS-CoV-2 and influenza viruses, are small RNA viruses, which means they are more nimble when it comes to mutating. But not mpox.
This means that even as mpox mutates, human T cells should still recognize some of the key epitopes that are “conserved,” or unchanged, between the original strain and the mutated clade 1 strain. “We expect that the majority of T cell epitopes will also be intact in the new strain,” says Sette.
The LJI team is now working to run bioinformatics analyses to examine genetic sequences from the mutated mpox virus and predict which epitopes have stayed the same. “The exact genome sequences for the new mpox strain are just now becoming available, and we will analyze them in the near future,” says Sette.
LJI labs study mpox patient samples
Sette and Grifoni are also analyzing valuable patient samples. “We are in a unique position to compare responses to different types of vaccines,” says Sette.
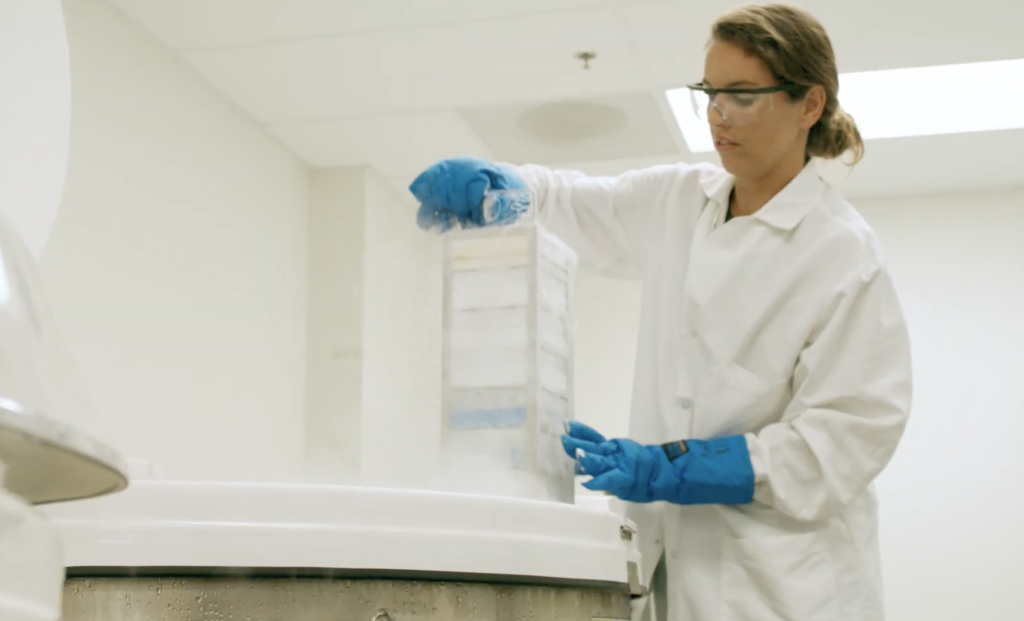
The researchers have access to clinical samples banked during a vaccine study conducted in the mid 2000s. This vaccine prompted T cells to recognize vaccinia virus, a kind of orthopoxvirus related to mpox and smallpox. This vaccine is not used today, but these banked samples give scientists an important window into how vaccines can trigger immune cell responses to mpox and related orthopoxviruses.
The LJI team is also working with human samples collected from infected and uninfected study participants during the 2022 mpox outbreak. Since then, these same individuals have returned to LJI to donate additional samples, which allows researchers to track the “durability” of mpox immunity and the effectiveness of the JYNNEOS and MVA vaccines over time.
“This access to samples—along with our ongoing vaccine research—puts us in a unique position to answer questions of how durable responses are after receiving two different vaccines or following infection,” Sette says. “These samples will also help us gain insights on how age and sex-based differences affect immune cell responses to mpox.”
Sette and Grifoni have also launched international collaborations to share mpox data as the virus mutates and spreads into different patient groups, including patients who are HIV positive.
LJI scientists win funding for pandemic preparedness
As members of the LJI Center for Vaccine Innovation, Sette and Grifoni lead innovative research to understand many pathogens with pandemic potential.
“We are studying which epitopes are conserved across entire viral families,” says Grifoni. “If we can identify the epitopes that different viruses have in common, we can be prepared no matter what these viruses throw our way.”
Sette and Grifoni have received significant funding from the National Institutes of Health, the SARS-CoV-2 Assessment of Viral Evolution (SAVE) consortium, the Coalition for Epidemic Preparedness Innovations (CEPI), and a private donor to investigate immune responses to emerging viruses with pandemic potential.
Importantly, the LJI Center for Vaccine Innovation has already developed a research pipeline that combines computational tools and with experimental data to uncover immune system targets for any virus of interest.
LJI scientists are currently applying this approach to many viral families of pandemic concern, including pox viruses, herpesviruses, arenaviruses (including Lassa virus), flaviviruses, paramyxoviruses, and influenza viruses including H5N1, a new highly pathogenic influenza strain that has been spreading worldwide since 2022.
Additional resources:
Sette Laboratory webpage
Grifoni Laboratory webpage
LJI Center for Vaccine Innovation