LA JOLLA, CA — Researchers at La Jolla Institute for Immunology (LJI) have at last uncovered how an enzyme called O-GlcNAc transferase (OGT) keeps cells healthy. Their findings, published in the Proceedings of the National Academies of Sciences, reveals a key aspect of cellular biology and may lead to important medical advances.
“Many diseases are related to OGT function,” says LJI Instructor Xiang Li, Ph.D., who served as first author for the new study. “For example, many studies have shown abnormal OGT function in cancer, diabetes, and cardiovascular disease.”
The new study, spearheaded by Li and co-led by LJI Professor Anjana Rao, Ph.D., and LJI Assistant Professor Samuel Myers, Ph.D., is the first to show that OGT controls cell survival by regulating a critical protein called mTOR.
Cells rely on mTOR to keep their mitochondrial powerhouses working. Without functional mTOR, cells fail at almost all their basic functions, from protein synthesis to cell proliferation. It’s not surprising that mTOR dysfunction is also a hallmark of many diseases.
“OGT is important for every cell in the body,” explains Myers. “Thanks to this research, we now have a model we can use for future studies into what each part of OGT does.”
The one and only OGT
OGT is an enzyme called a transferase. This type of enzyme carries out a job called glycosylation, where sugar molecules are added to recently synthesized proteins. OGT is unique among transferases because it modifies proteins within cells, rather than proteins on the cell surface or secreted proteins.
In fact, OGT’s job of glycosylation is so important that embryonic cells will die without it. But until now, scientists were in the dark as to why.
As Myers explains, the essential nature of OGT is what makes it so hard to study. Scientists usually study enzymes and other proteins by developing cells that lack the genes for those proteins. They generate the new, dysfunctional cells and then investigate how things have gone wrong.
But with OGT, that kind of experiment would be over before it even began. Because there is only one OGT, scientists haven’t been able to delete it or reduce its function without simply killing the very cells they need to study. “We knew OGT was essential for cell survival, but for more than 20 years we didn’t know why,” says Li.
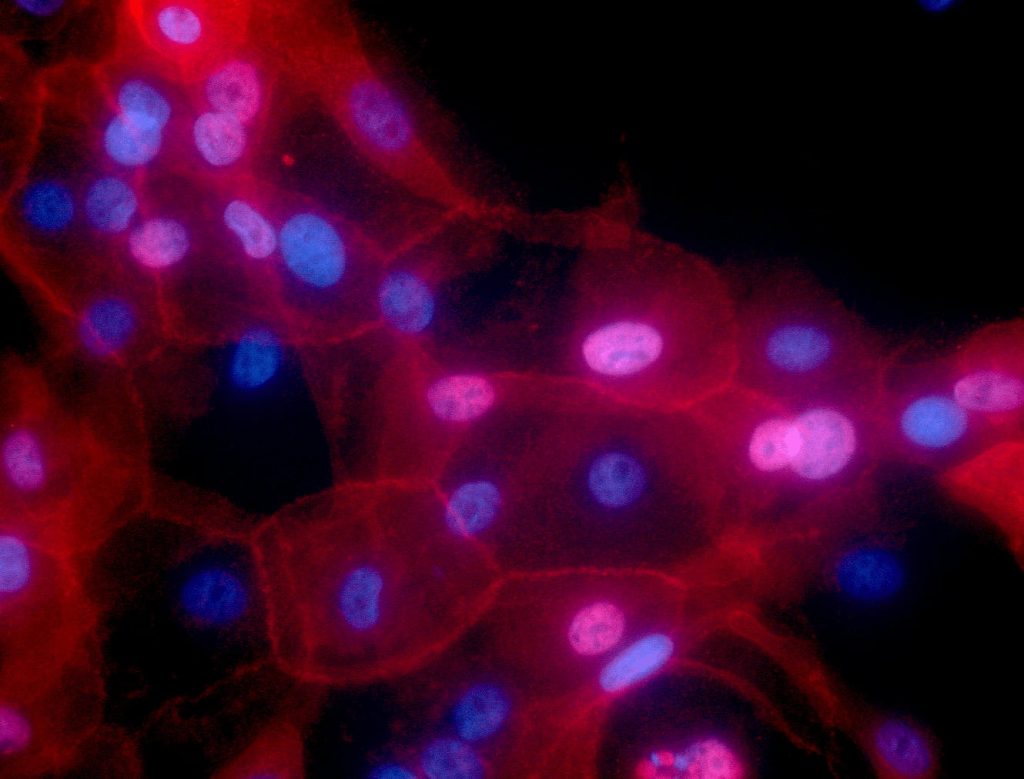
For the new study, Li was able to get around that problem by using an inducible system to delete the OGT gene. He worked with mouse embryonic stem cells and then used an inducible version of a protein known as Cre to delete the gene for OGT. This meant that the cells could grow normally until the scientists decided to activate the process, after which cells that had lost the OGT gene began to stop proliferating and die.
The team found that deleting the gene for OGT led to an abnormal increase in the function of a key enzyme called mTOR that regulates cell metabolism. Deleting the gene for OGT also fueled an essential but potentially dangerous process in cells called mitochondrial oxidative phosphorylation.
Why is mitochondrial oxidative phosphorylation so dangerous? This process in cells is part of a delicate pathway that allows cells to produce ATP (the molecule that powers a cell). ATP can be produced by glycolysis as well as by mitochondrial oxidative phosphorylation, and disturbing this balance can have devastating consequences for cells.
Fortunately, OGT safeguards mTOR activity and mitochondrial fitness by keeping protein synthesis running smoothly and regulating amino acid levels within cells. Importantly, the researchers discovered the same protective role for OGT in CD8+ T cells, which suggests the enzyme works the same way across mammalian cell types, not just in mouse embryonic stem cells.
Researchers to the rescue
Even the dysfunctional cells lacking OGT weren’t doomed forever. The scientists were able to “rescue” the dysfunctional cells using a new cutting-edge technology for gene editing called CRISPR/Cas9.
By asking whether a second gene in the mouse embryonic stem cells would restore the growth of cells lacking OGT, Li found that mTOR and mitochondrial oxidative phosphorylation were hyperactivated in cells lacking OGT, and the cells could be rescued by damping down their function.
This is good news for scientists hoping to learn more about OGT’s role in the body. “Now that we can delete the gene for OGT while keeping cells alive, we can try restoring just pieces of OGT to learn more about how OGT works to keep cells alive,” says Myers.
Li says his new discovery may allow researchers to further study the role of OGT and potentially find therapeutic targets to counteract abnormal activity. “In the future, we hope our research could help shed light on issues related to dysfunctional OGT in cancer and other diseases,” Li says.
Additional authors of the study, “OGT controls mammalian cell viability by regulating the proteasome/mTOR/mitochondrial axis,” include Xiaojing Yue, Hugo Sepulveda, Rajan A. Burt, David A. Scott, and Steven A. Carr.
The study was supported by the National Institutes of Health (R01 grants R35 CA210043 and R01 CA247500; Shared Instrumentation Grant Program grants S10 RR027366 and Hiseq 2500 S10OD016262), the NCI Cancer Center (support grant P30 CA030199), a postdoctoral Fellowship from CIRM UCSD Interdisciplinary Stem Cell Research & Training Grant II (TG2-01154), and through the Pew Latin American Fellows Program from the Pew Charitable Trusts.
###





