LA JOLLA, CA—Scientists at La Jolla Institute for Immunology (LJI) have uncovered the structure and function of the first FDA-approved treatment for Zaire ebolavirus (Ebola virus).
Inmazeb (REGN-EB3), developed by Regeneron, is a three-antibody cocktail designed to target the Ebola virus glycoprotein. The drug was first approved for clinical use in October 2020, but its exact mechanism of action has remained unclear.
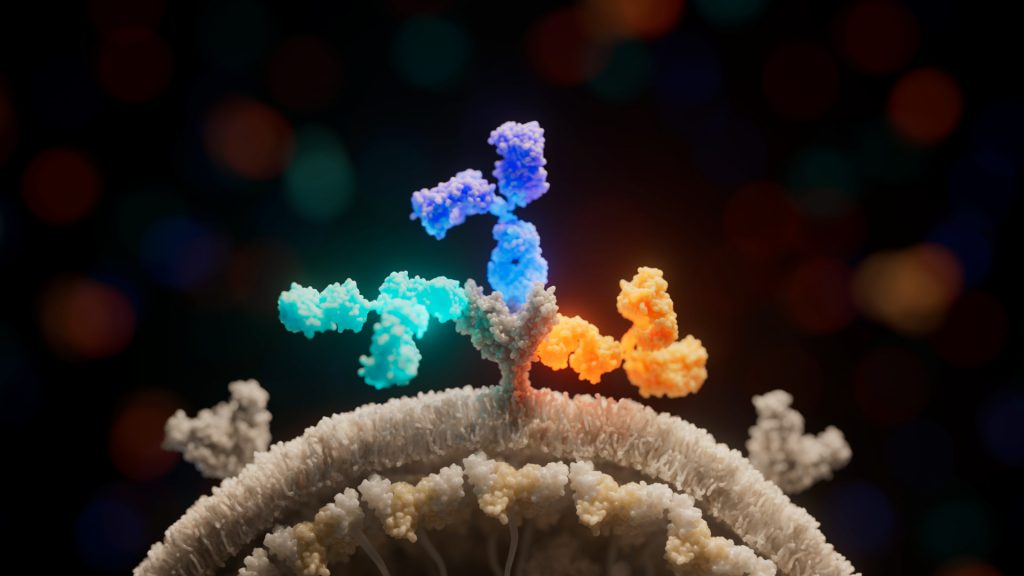
In the cover story of the latest issue of Cell Host & Microbe, LJI researchers present a high-resolution, 3D structure of the three antibodies as they bind to the Ebola virus glycoprotein (the viral protein that launches Ebola virus infection). The model reveals new information about both the drug and the virus, and how their interaction fights infection and protects against future viral mutations.
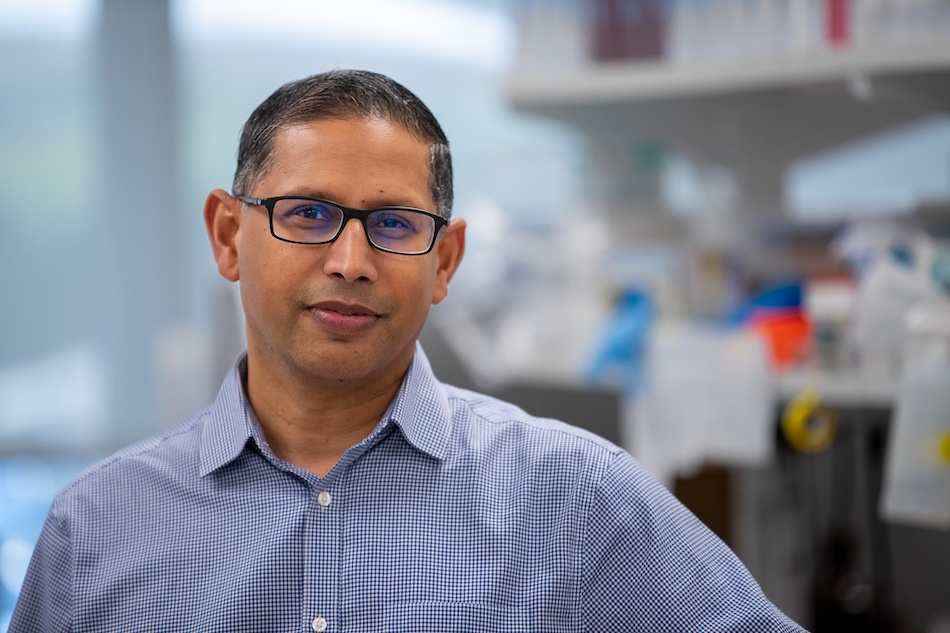
“Before this, we had a general idea of what the drug was doing, but we didn’t know exactly how,” says LJI President and CEO Erica Ollmann Saphire, Ph.D., who served as senior author of the study. “We now know which specific amino acids the antibodies are latching onto and how their binding affects the viral glycoprotein.”
The new research also shows the potential for Inmazeb in treating additional species of Ebolavirus.
How the antibody cocktail works
At 3.1 angstroms, the 3D structure is the highest-resolution image of the Ebola virus surface protein ever assembled using asymmetric reconstruction. The researchers achieved this detailed view through an imaging technique called cryogenic electron microscopy (cryo-EM).
“It’s like getting mugshots of a protein,” said first author Vamseedhar Rayaprolu, Ph.D., who spearheaded the project as a postdoctoral associate at LJI and now serves at The Pacific Northwest Center for Cryo-EM. “We take photos of the complex that is frozen in all different angles and then stitch them together to get a 3D model.”
Thanks to these images, the LJI team immediately made a discovery not just about the drug, but also about Ebola virus itself. While the overall structure of the Ebola glycoprotein has been known for some time, one region had yet to be modeled effectively—the β17-β18 loop on the protein’s glycan cap.
“This piece is normally too floppy to be imaged,” said Rayaprolu, “but when the antibodies were bound to the virus, they locked the loop into place and we were able to finally capture its location and structure.”
The team then confirmed that the drug’s three antibodies bind the glycoprotein at distinct, non-overlapping locations, maximizing their effectiveness by minimizing their redundancy.
Atoltivimab (REGN3470) is the specific antibody that binds the β17-β18 loop. When bound, this antibody can serve as a signal to attract the immune system, flagging infected cells to be killed via effector functions.
A second antibody, called odesivimab (REGN3471), binds to amino acids on the glycoprotein’s receptor-binding site, preventing the virus from attaching itself to human cells.
The third antibody, called maftivimab (REGN3479), binds and warps the glycoprotein’s internal fusion loop, which the virus requires to drive itself into a cell. The researchers also found evidence that maftivimab may be valuable in future therapies against other types of Ebolaviruses.
Fighting more than one virus
“Like with SARS-CoV-2, Ebola virus has changed over time and become different than the original virus,” says study collaborator Robert Davey, Ph.D., Professor in the National Emerging Infectious Diseases Laboratories (NEIDL), of the Boston University Chobanian & Avedisian School of Medicine. As Davey points out, Ebola viruses aren’t the only dangerous members of the larger Filovirus family. This family includes closely related Ebolavirus species, such as Sudan ebolavirus (a 2022 outbreak of Sudan ebolavirus killed at least 55 people in Uganda) and the more distantly related Marburg virus.
Through a series of escape studies led by study collaborators in Davey’s lab and at Regeneron, the team found that Inmazeb could potentially protect against several viruses in the Ebolavirus genus of Filoviruses, including Sudan ebolavirus.
The key appears to be the maftivimab antibody. Maftivimab’s target, the viral glycoprotein’s internal fusion loop, is conserved across these Ebolaviruses. This means the loop structure has not changed significantly, even as other parts of the virus have mutated over time.
“We found that, in general, the antibodies in Inmazeb could be effective against the more closely related viruses,” says Davey. “But for the more distantly related species, such as Marburg, more work needs to be done to devise a new antibody cocktail.”
Could Inmazeb also combat new Ebola virus variants? The researchers found that—in the presence of all three antibodies—Ebola virus has to undergo ten rounds of replication and multiple mutations to partially escape the effects of the drug. In contrast, using any single antibody alone leads to escape mutations within only one or two passages.
This finding suggests that Inmazeb can provide lasting immunity against variants. The new findings may also guide the development of novel antibody drugs that target the glycoprotein more broadly or effectively.
“We now understand how subtle shifts in the landing site of different antibodies impact function,” says Rayaprolu. “This tells us the differences between more or less effective immune responses.”
“Knowing exactly where a drug contacts the virus helps us predict whether it is likely to still work on a new viral variant,” adds Saphire. “These methods and the insights from our research collaborators will be integral to the development of next-generation vaccines.”
Additional authors of the study, “Structure of the Inmazeb cocktail and resistance to Ebola virus escape,” include Benjamin O. Fulton, Ashique Rafique, Emilia Arturo, Dewight Williams, Chitra Hariharan, Heather Callaway, Amar Parvate, Sharon L. Schendel, Diptiben Parekh, Sean Hui, Kelly Shaffer, Kristen E. Pascal, Elzbieta Wloga, Stephanie Giordano, Nicole Negron, Min Ni, Richard Copin, Gurinder S. Atwal, Matthew Franklin, Ruth Mabel Boytz, Callie Donahue, Robert Davey, Alina Baum, and Christos A. Kyratsous, researchers at Regeneron, Boston University and La Jolla Institute for Immunology.
The study was supported by the NIH National Institute of Allergy and Infectious Diseases (grant U19 AI142790), the Consortium for Immunotherapeutics against Emerging Viral Threats, and the U.S. Department of Health and Health Services Contract No. HHSO100201700016C (Regeneron). Additional funding was provided by the Department of Health and Human Services, the NIH National Cancer Institute (grant ACB-12002), and the NIH National Institute of General Medical Sciences (grants AGM-12006 and P30GM138396).
DOI: 10.1016/j.chom.2023.01.002
###