LA JOLLA, CA—Scientists at La Jolla Institute for Immunology (LJI) have developed six lines of humanized mice that can serve as valuable models for studying human cases of COVID-19.

According to their new study in eBioMedicine, these mouse models are important for COVID-19 research because their cells were engineered to include two important human molecules that are involved in SARS-CoV-2 infection of human cells—and these humanized mice were generated on two different immunologic backgrounds. The new models can help shed light on how SARS-CoV-2 moves through the body and why different people experience wildly different COVID-19 symptoms.
“With these mouse models, we can model epidemiologically-relevant SARS-CoV-2 infection and vaccination settings, and we can study all relevant tissues (not just the blood) at different timepoints following infection and/or vaccination,” says LJI Professor Sujan Shresta, Ph.D., who co-led the research with LJI Histopathology Core Director Kenneth Kim, Dipl. ACVP, and the late Kurt Jarnagin, Ph.D., of Synbal, Inc.
Already, these new mouse models have helped scientists capture a clearer picture of how SARS-CoV-2 affects humans. They are also available to the wider COVID-19 research community.
“This work is part of LJI’s mission to contribute to pandemic preparedness around the world,” says Shresta.
Mouse models are a critical tool for understanding infection
Shresta’s lab is known for producing mouse models to study immune responses to infectious diseases such as dengue virus and Zika virus. In 2021, her laboratory partnered with Synbal, Inc., a preclinical biotechnology company based in San Diego, CA, to develop multi-gene, humanized mouse models for COVID-19 research. The project was also supported by Synbal CEO and LJI Board Member David R. Webb, Ph.D.
Shresta and Jarnagin collaborated to produce mice that express either human ACE2, human TMPRSS2, or both molecules in the C57BL/6 and BALB/c mouse genetic backgrounds. “Immunologists have found that these two genetic backgrounds in mice elicit different immune responses,” says Shresta.
As Shresta explains, having the flexibility to include the genes for one or both of these molecules in two different mouse genetic backgrounds gives scientists an opportunity to investigate two key areas. First, they can examine how each of these molecules contribute to infection with different SARS-CoV-2 variants. Second, they can study how the host’s genetic background might influence disease progression and immune response following infection with different variants.
Zooming into infected tissues
The researchers then took a closer look at how these models responded to actual SARS-CoV-2 infection. LJI Postdoctoral Fellow Shailendra Verma, Ph.D., worked in LJI’s High Containment (BSL-3) Facility to take tissue samples from the various mouse strains exposed to SARS-CoV-2.
“This work wouldn’t have been possible if we didn’t have a BSL-3 facility at LJI,” says Shresta, who has worked closely with LJI’s Department of Environmental Health and Safety to conduct several cutting-edge studies in the facility.
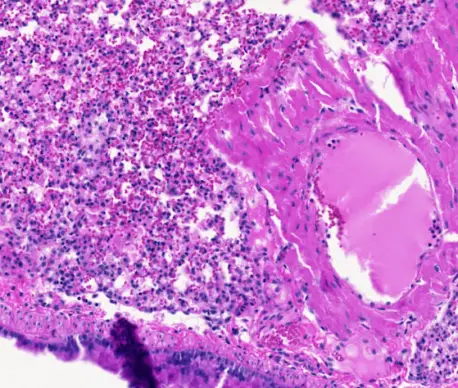
Next, Kim, a board-certified pathologist, examined the tissue samples and compared them to pathologic findings from humans with COVID-19. Kim’s analysis showed signs of SARS-CoV-2 infection in the lungs, which are also the tissue most vulnerable to SARS-CoV-2 infection in humans. Kim could also see mouse immune cells responding to infection in a way that reflected the human immune response.
By characterizing these responses in the new mouse models, the researchers have established a foundation for understanding the immune heterogeneity—or wide range of immune responses—of SARS-CoV-2-induced disease.
“There’s no such thing as a perfect animal model, but our goal is always to make an animal model that recapitulates the human disease and immune response as much as possible,” says Shresta.
The new mouse models may prove valuable for studying responses to emerging SARS-CoV-2 variants and future coronaviruses with pandemic potential.
“Not only are these models useful for current COVID-19 studies, but if there should be another coronavirus pandemic—with a virus that utilizes the same ACE2 receptor and/or TMPRSS2 molecule for viral entry into human cells—then these mouse lines on two different genetic backgrounds will be ready,” says Kim.
Additional authors of the study, “Influence of Th1 versus Th2 immune bias on viral, pathological, and immunological dynamics in SARS-CoV-2 variant-infected human ACE2 knock-in mice,” include Erin Maule, Paolla B. A. Pinto, Chris Conner, Kristen Valentine, Dale O Cowley, Robyn Miller, Annie Elong Ngono, Linda Tran, Krithik Varghese, Rúbens Prince dos Santos Alves, Kathryn M. Hastie and Erica Ollmann Saphire.
This study was supported by the National Institutes of Health (grant U19 AI142790-02S1 and R44 AI157900), the GHR Foundation, the Arvin Gottlieb Charitable Foundation, the Overton family, and by a American Association of Immunologists Career Reentry Fellowship (FASB).
DOI: 10.1016/j.ebiom.2024.105361
###