LA JOLLA, CA—Your gut is a battleground. The cells that line your small intestine have to balance two seemingly contradictory jobs: absorbing nutrients from food, while keeping a wary eye out for pathogens trying to invade your body.
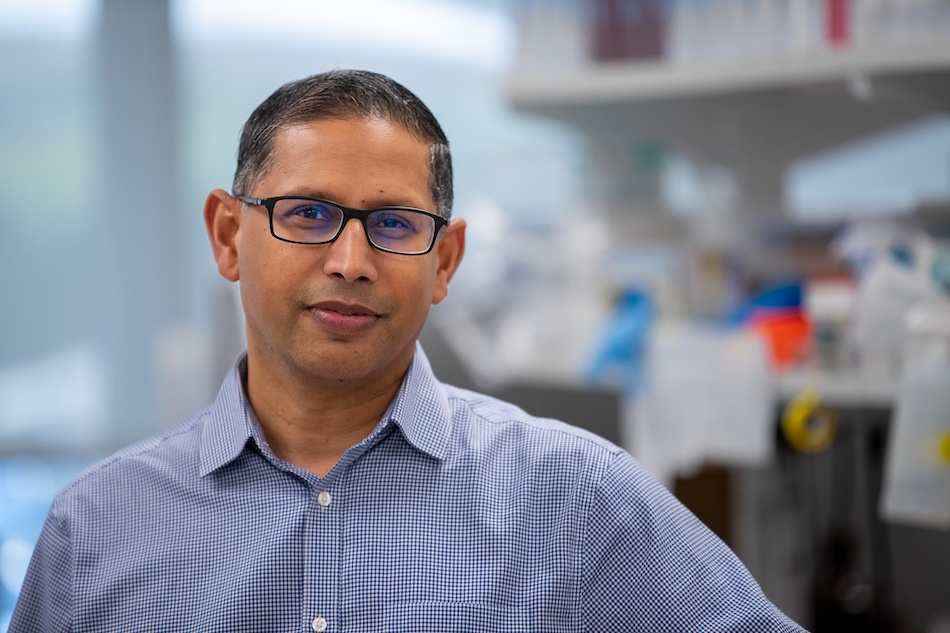
“This is a surface where pathogens can sneak in,” says La Jolla Institute for Immunology (LJI) Assistant Professor Miguel Reina-Campos, Ph.D. “That’s a massive challenge for the immune system.”
So how do immune cells keep the gut safe? New research led by scientists at LJI, UC San Diego, and the Allen Institute for Immunology shows that pathogen-fighting immune cells called tissue-resident memory CD8 T cells (TRM cells) go through a surprising transformation—and relocation—as they fight infections in the small intestine.
In fact, these cells literally rise up higher in the tissue to fight infections before pathogens can spread to deeper, more vulnerable areas.
“The tissue in the gut has evolved to provide signals to immune cell infiltrates—to put immune cells in specific places so they have a better ability to stop pathogens,” says Reina-Campos, who served as first author of the new Nature study alongside co-first author Alexander Monell of UC San Diego and co-senior authors Maximilian Heeg, M.D., and Ananda W. Goldrath, Ph.D., of the Allen Institute for Immunology and UC San Diego.
The new findings add to the growing body of evidence that immune cells adapt to protect specific tissues. Reina-Campos thinks these “tissue-resident” immune cells may be key players in future cancer immunotherapies that target tumors in specific organs.
T cells on the move
Reina-Campos and his colleagues investigated the formation of TRM cells in the small intestine. The team harnessed a cutting-edge technology called spatial transcriptomics to track these cells in both human and mouse tissue samples.
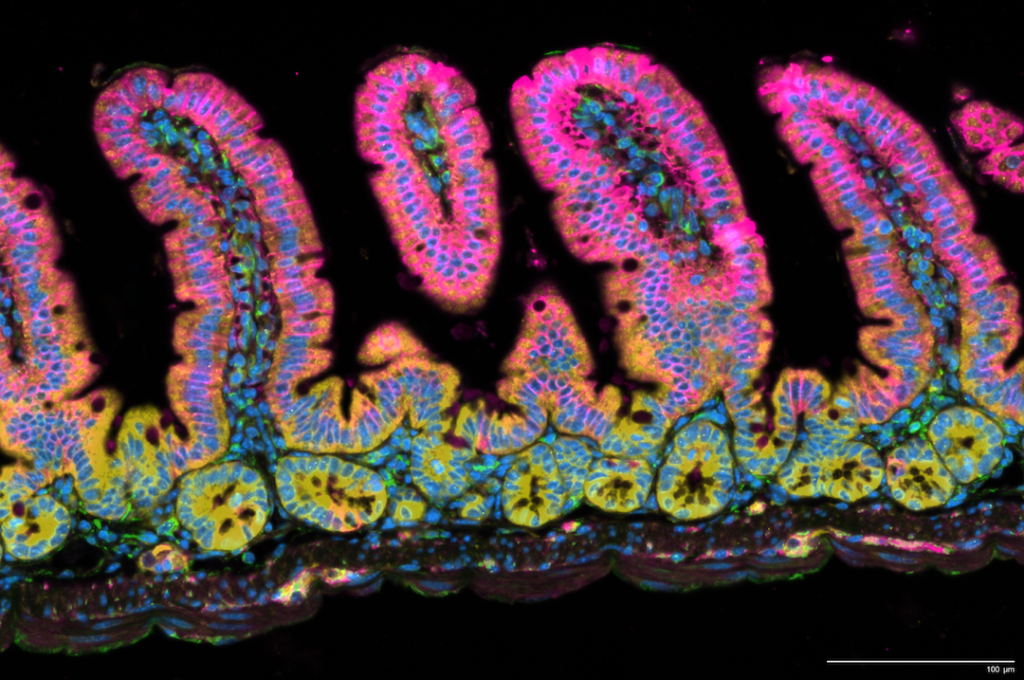
Their work showed that the small intestine holds two types of TRM cells. These cells are split between the tiny, finger-like “villi” structures that line the small intestine or the “crypts” between the protruding villi.
The researchers found that progenitor-like TRM cells live closer to the crypts between the villi. On the other hand, differentiated TRM occupy more exposed regions at the top of the villi. “Differentiated immune cells are more exposed at the top of the villi, and that’s where they have a better ability to protect you from infections,” says Reina-Campos.
Meanwhile, a reserve population of progenitor-like TRM cells continues to lie low in the crypts. “These cells can replenish the pool of effector T cells, so the immune system keeps them as back-ups in the deeper parts of the tissue,” adds Reina-Campos.
What keeps these populations organized and in check?
To spy on these important immune cells within their natural habitat, Reina-Campos and colleagues used a new technology—called spatial transcriptomics—to observe millions of messenger RNA molecules simultaneously at subcellular resolution.
“For the first time, we were able to capture the formation of immunological memory in space and time,” says Reina-Campos.
Looking at small intestines after a viral infection, the scientists found that the gut releases chemical signals to instruct immune cells where to go and what to do. “This study offers a new resource for finding signals that position immune residents to strengthen our gut immunity,” says Reina-Campos.
Checkmate for disease?
Reina-Campos credits his mentor, Goldrath, as well as Heeg’s and Monell’s expertise for making this study possible. As Reina-Campos explains, Heeg and Monell developed new computational approaches to make sense of the massive amounts of data captured through spatial transcriptomics.
“It’s led to a breakthrough in our ability to look at hundreds to thousands of genes simultaneously in intact tissues,” says Reina-Campos. “With this study, we’ve opened up a new path for discovery.”
Reina-Campos compares the battle between immune cells and pathogens to a chess match.
“To be a chess grandmaster, you need to know not only about the pieces: the bishops, pawns, rooks, etc, but also how they move in concert on the chessboard,” he says.
For a long time, scientists have studied the chess pieces—by analyzing cells extracted from tissue—but they haven’t gotten a good look at the chess match itself. “We don’t know as much about how the chessboard works—and we know even less about the rules that apply to our chess pieces as they move across the board,” says Reina-Campos.
The new study gives researchers a detailed look at how immune cells interact with each other and their cellular gameboard.
Reina-Campos says the new finding should guide future research into how immune cells develop and move through other organs with different tissue structures, such as the kidneys and lungs—and how immune cells might fight tumors in these organs.
Additional authors of the study, “Tissue-resident memory CD8 T cell diversity is spatiotemporally imprinted,” include Amir Ferry, Vida Luna, Kitty P. Cheung, Giovanni Galletti, Nicole E. Scharping, Kennidy K. Takehara, Sara Quon, Peter P. Challita, Brigid Boland, Yun Hsuan Lin, William H. Wong, Cynthia S. Indralingam, Hayley Neadeau, Suzie Alarcón, Gene W. Yeo, and John T. Chang.
The study was supported by the National Institutes of Health (grants R01AI179952, R37AI067545, P01AI132122, R01AI072117, R01AI150282, R01CA273432, S10OD025052, and F31AI176705), NIDDK-funded San Diego Digestive Diseases Research Center (P30DK120515), U.S. Department of Veterans Affairs CRSD Service (I01 CX002396), NINDS (P30NS047101), a NCI Predoctoral to Postdoctoral Fellow Transition (F99/K00) Award (K00CA222711), a Canadian Institutes of Health Research Doctoral Foreign Study Award, and a Cancer Research Institute Postdoctoral Fellowship (CRI4145).