Zika has been declared an international health emergency by the World Health Organization citing concerns that as many as four million people could be infected by the end of 2016. Several LJI labs have joined the worldwide effort to combat Zika.
Zika virus causes mild symptoms in most people, including fever, headache, rash, and possibly pink eye. In fact, most individuals never realize they have been infected. That is especially concerning for pregnant women as they unknowingly may pass on the virus to their unborn babies where it can cause severe developmental disorders and even death.
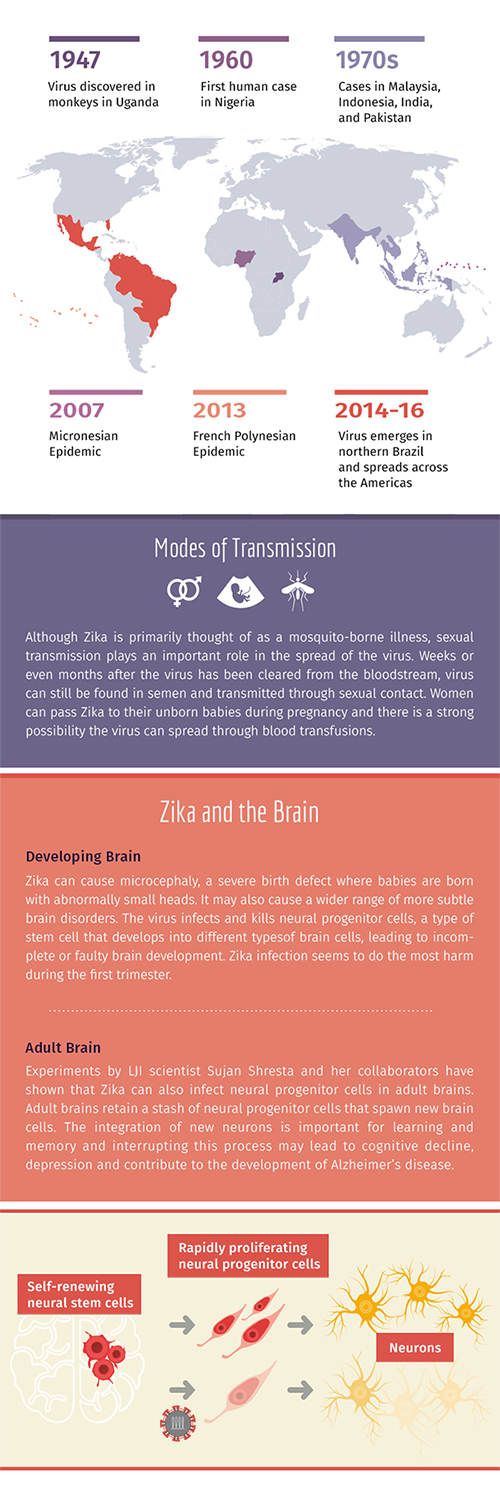
As the epidemic progresses, more complications related to Zika infection are emerging. We now know that in addition to causing eye damage in babies, adults’ vision can be affected as well. Babies that appear healthy at birth are sometimes coming down with microcephaly and other brain-related disorders months after birth.
In response to the recent Zika outbreak, several LJI scientists recently shifted their focus to Zika research. Their efforts involve a network of scientists from Florida, North Carolina, Nicaragua, Colombia, and Brazil and tie in with a large Zika research project sponsored by the European Union.
Dr. Sujan Shresta, who is internationally recognized for her pioneering work on dengue virus, developed a Zika mouse model that can mimic the virus infection in the lab. She is particularly interested in learning how the virus spreads and evades the immune system as well as in screening vaccine candidates and compounds that can treat Zika infections. The mouse model also formed the basis for studying the virus’ effect on adult brain cells (see “Zika and the brain”).
Dr. Alessandro Sette, known for his work studying the role of T cells in the immune response to other flaviviruses, such as dengue and yellow fever, is also expanding the scope of his research to include Zika. He is particularly interested in whether dengue infections or yellow fever vaccinations crossreact with Zika infections.
In collaboration with Dr. Bjoern Peters’ lab, his team is identifying those parts of the virus particle that are recognized by the immune system. It is an extension of Dr. Peters’ most recent study, which used machine- learning tools to predict which parts of Zika are likely to elicit an immune response.
Together with experimental data, this research not only provides the basis to map how the human immune system responds to Zika and what makes some people more resistant to disease but also how to best measure the efficacy of vaccine candidates.

